Jump to topic
Search
Program Details
The Pediatric Residency at Penn State Health Children’s Hospital features a balanced and individualized training curriculum executed in a supportive and resident-driven learning environment.
The program is ideally sized to offer a family-like atmosphere but also flexibility for time off. As the only children’s hospital, pediatric intensive care unit and Level IV neonatal intensive care unit in the region, Penn State Health Children’s Hospital offers a level of patient diversity, acuity and complexity that is comparable to, and may exceed that of, the largest children’s hospitals and pediatric residency programs in the nation.
Learn More about the Residency
Thank you for your interest in the Pediatric Residency at Penn State Health Children’s Hospital.
Our program prides itself on helping trainees develop the lifelong skills of goal-setting and self-directed learning within a curriculum that allows significant flexibility for individualization. The ACGME is requiring an extensive individualized curriculum for each pediatric residency program in 2025, but our residency has been implementing this educational innovation for over a decade. Our residents are the driving force not only of their own professional development, but also in the continued evaluation and improvement of the residency experience with opportunities to participate in numerous committees focused on wellness, curriculum development, program evaluation, recruitment, patient safety, quality improvement, informatics and diversity, equity and inclusion.
Trainees are also given the opportunity to further develop their educator skills through lectures, electives and retreats offered by the Woodward Center for Excellence in Health Sciences Education. No matter your interest, we will work hard to find educational opportunities to support your goals.
This is an exciting time to join the Penn State Health pediatric family. Penn State Health Children’s Hospital’s specialties have been ranked by the U.S. News and World Report every year for the last 13 years, consistently placing it as a top 20 Children’s Hospital in the Mid-Atlantic Region. Our Children’s Hospital has recently expanded, now featuring a new, 56-private-bed NICU; Labor and Delivery and postpartum area; and post-surgical acute-care unit. We have also recently acquired the Pennsylvania Psychiatric Institute (PPI) in nearby Harrisburg to provide comprehensive mental health services to our patients and opened up regional pediatric medical centers in Lancaster and Harrisburg, PA.
The town of Hershey, located 13 miles from the state capital of Harrisburg, is an easy and affordable place to live, where residents are able to rent apartments or purchase homes in safe neighborhoods with highly rated public schools all within a few miles of the hospital. Whether you want to ride one of the 15 roller coasters at Hersheypark, catch a concert at Hersheypark Stadium, laugh with your favorite comedian at the Giant Center, watch a musical at the Hershey Theater, cheer on the Hershey Bears hockey team (2023 Calder Cup Champions!), kayak the Swatara Creek/Susquehanna River, hike the Appalachian Trail, bike the Capital Area Greenbelt, or relax at a local winery/brewery, there is something in this region for everyone.
The Harrisburg/Hershey area is ranked 38th in the 2023 U.S. News “Best Places to Live” rankings. It is also within a short day’s trip to many major cities and attractions such as Baltimore (90 miles), Philadelphia (95 miles), Poconos Mountains (110 miles), Washington DC (135 miles), Shenandoah National Park (150 miles), New York City (160 miles), and Pittsburgh (215 miles). Learn more about the Hershey area here.
Additionally, historical Lancaster City is located only 40 minutes east of Hershey Medical Center. It has a vibrant art scene with local artists and unique antiques and offers Broadway-caliber shows at the Fulton Theater – a beautifully restored 165-year-old national historic landmark of ornate Victorian architecture.
This is an exciting time to live and train in central Pennsylvania at Penn State Health Children’s Hospital, and we hope you consider joining us!
Aaron R. Shedlock, MD, FAAP
Program Director, Pediatric Residency
The mission of the program is to recruit a diverse residency cohort, support each resident’s learning needs with respect to background and experiences, and provide education and opportunities that teach residents excellence in clinical care, community health, advocacy, quality improvement and innovative medical research. Residents will graduate from this program as highly-qualified pediatricians capable of navigating the healthcare system and providing evidence-based, personalized and culturally responsive care to a diverse group of patients.
The aims of the program are to foster an inclusive, supportive, and personalized learning environment in which each resident:
- Acquires the skills, knowledge and confidence needed to be a general pediatrician who holistically cares for the physical and mental health of children with respect to principles of diversity, equity, inclusion, cultural humility, social determinants of health and healthcare disparities.
- Develops the skills necessary to be a successful lifelong self-directed learner.
- Sets and achieves their own individualized learning objectives and curricula to satisfy educational and career goals.
- Utilizes the support of coaches, mentors and program leaders to meet their individualized objectives and goals.
- Receives the flexibility and support, and is taught the skills necessary, to achieve and maintain their wellness needs.
- Participates in program evaluation and has a voice in creating strategic changes.
The program’s educational philosophy recognizes that each resident:
- Enters training with a unique array of knowledge, skills, attitudes and interests
- Develops along an individual trajectory toward competency
- Has specific personal and professional goals to achieve during residency
The curricular philosophy is to provide an appropriate balance between:
- General pediatric training and subspecialty training
- The inpatient setting and the outpatient setting
- Supervision and autonomy
- Personal responsibility/ownership and shared responsibility/teamwork
- Experiential learning and formalized classroom learning
- A mandatory curriculum and an individualized curriculum
- Time spent working and time spent thinking and reflecting
- The necessary rigors of residency and the promotion of resident wellness
The operational philosophy is that residents:
- Play a critical role in a constant cycle of program re-evaluation and improvement
- Are a leading voice in the evolution of the program over time
- Have a sense of ownership of the program
General Application Information
All applicants must apply through the Electronic Residency Application Service (ERAS) by Dec. 1 and must register for a PL-1 position through the National Resident Matching Program (NRMP).
Applications are considered without regard to age, color, disability, gender identity or expression, marital status, national or ethnic origin, political affiliation, race, religion, sex (including pregnancy), sexual orientation, veteran status and family medical or genetic information. The program sponsors J-1 visas only. Current or recent experience working in the U.S. healthcare system is strongly preferred.
For the 2023-2024 ERAS® cycle, this program is participating in the supplemental ERAS application program signaling process.
Learn more about the AAMC supplemental ERAS application.
Applicants who are offered interviews, match into the Pediatrics residency program, and successfully complete the residency, will be deemed board eligible for certification by the American Board of Pediatrics. Please refer to the American Board of Pediatrics website for additional information.
Application Requirements
- Personal statement
- MSPE (dean’s letter)
- Medical school transcript
- USMLE or COMLEX scores
- Three to four letters of recommendation from faculty members with whom the applicant has worked
The program does not require a letter from the applicant’s department chair or clerkship director.
Interview Process
Interviews are by invitation only, and will be conducted from late-October through December.
All interviews will be conducted virtually during the 2023-2024 application cycle as recommended by the Association of Pediatric Program Directors (APPD), COMSEP and AAMC.
The virtual interview day schedule will be approximately 4 hours long and include:
- Introduction to the program (with program leadership)
- Interviews with program leadership and faculty
- “Life as a Resident” Q&A/Virtual Tour with Chief Residents
- Program director question-and-answer session/wrap-up
An optional virtual social hour with residents will be arranged the night before your interview by the recruitment committee as well.
Program Leadership
Coaching Program Overview
Trainees are paired with one of seven expert coaches who are specially trained and provided protected time to help facilitate and monitor clinical/academic progression, goal-setting, career planning and wellness throughout the entire residency.
Housestaff sessions are also scheduled every 2-4 weeks with the residents and program leadership (program directors, chiefs and coordinators) to provide ongoing support.
- Continuity clinic preceptor – every week
- Chief residents – early in the fall of intern year
- Coach – three times a year
- Program director/associate program directors – twice yearly
- Director of individualized education – each winter (to choose electives)
- Chair of Pediatrics – once a year over lunch
Housestaff sessions are also scheduled every 2-4 weeks with the residents and program leadership (PD, chiefs and coordinators) to provide ongoing support.
Coaches

Pediatric and Medicine-Pediatrics interns participated in the residency program’s annual intern retreat at the Englewood in Hershey.
Dr. Angel Schuster, associate program director of the Pediatric Residency and vice chair of DEI for the Department of Emergency Medicine, presents “Diversity is Important, Knowing Your Co-Workers” at the intern retreat.
Christine Irvin, associate program director of the Pediatric Residency, and Laura Keefer, associate program directory of the Internal Medicine/Pediatric Residency, present “Manage Up” at an intern retreat.

From left, pediatric interns Luke Avenel, Kim Benson, Marie Schwalbe and Sarah Houseal participate in a Scavenger Hunt during orientation and take a photo with Penn State’s mascot, the Nittany Lion!

From left, pediatric interns Catherine Hercules, Tom Barrett, Lauren Andree, and Elise Quinn get their Nittany Lion photo during the scavenger hunt.
Stay in touch
Program graduates are asked to update information to remain on the program’s mailing list.
Five-year resident placements (2019 to 2023)
pursued fellowship
entered general pediatrics
took another path
(additional residency, chief year outside the organization, etc.)
entered hospital medicine
Past Resident Listing
Residents from this program have gone on to fellowship at a variety of academic medical centers across the country. Use the search bar above the photo grid to see specific locations and subspecialties for these graduates.
ACADEMIC GENERAL PEDIATRICS
Nemours Children’s Health
ALLERGY & IMMUNOLOGY/PEDIATRICS
Johns Hopkins Children’s Center
NEONATOLOGY
University of Rochester Medical Center
PEDIATRIC CARDIOLOGY
University of Texas Health
PEDIATRIC CRITICAL CARE MEDICINE
University of Alabama Birmingham Medical Center
PEDIATRIC EMERGENCY MEDICINE
Northwell Cohen Children’s
Children’ Hospital of the King’s Daughters (EVMS)
PEDIATRIC HOSPITAL MEDICINE
UCLA Medical Center
PEDIATRIC INFECTIOUS DISEASE
University of Pittsburgh Medical Center
PEDIATRIC PULMONOLOGY
University of Texas Health
PEDIATRIC RHEUMATOLOGY
Northwell Cohen Children’s
Academic General Pediatrics
- Boston Children’s Hospital
Allergy & Immunology/Pediatrics
- Johns Hopkins Children’s Center
Pediatric Critical Care Medicine
- University of Miami/Jackson Health System
- University of Rochester/Strong Memorial Hospital
- Johns Hopkins Hospital
- Case Western/University Hospital Cleveland Medical Center
Pediatric Hospital Medicine
- UCLA Medical Center
Developmental-Behavioral Pediatrics
- Brown University/Rhode Island Hospital
Neonatal/Perinatal Medicine
- Children’s Hospital of Michigan
- Penn State Milton S. Hershey Medical Center
Pediatric Critical Care Medicine
- Johns Hopkins All Children’s Hospital
Pediatric Emergency Medicine
- Children’s Hospital of Michigan
- Phoenix Children’s Hospital
- University of North Carolina Hospitals
- Wright State University Boonshoft School of Medicine
Pediatric Hematology/Oncology
- Children’s National Medical Center
- Northwestern McGaw/Lurie Children’s Hospital
- Phoenix Children’s Hospital
Pediatric Urgent Care
- Children’s National Medical Center
Sports Medicine
- Children’s Hospital of Philadelphia
Neonatal/Perinatal Medicine
- University of Rochester
Pediatric Cardiology
- Mount Sinai
Pediatric Critical Care Medicine
- Rainbow Babies and Children’s Hospital
- Riley Children’s Hospital
Pediatric Emergency Medicine
- Baystate Medical Center
Pediatric Hospital Medicine
- University of Florida – Jacksonville
Pediatric Neurodevelopmental Disabilities Residency
- Johns Hopkins University
Sports Medicine, Pediatric Track
- University of Colorado
Allergy/Immunology
- Penn State Milton S. Hershey Medical Center
Neonatal/Perinatal Medicine
- Stony Brook Children’s Hospital
Pediatric Critical Care Medicine
- Loma Linda University Children’s Hospital
- Nationwide Children’s Hospital (2)
Developmental-Behavioral Pediatrics
- Prisma Health, Greenville Health Systems
Pediatric Cardiology
- Penn State Milton S. Hershey Medical Center
- University of Utah
Pediatric Critical Care Medicine
- Duke University
- Johns Hopkins All Children’s Hospital
Pediatric Gastroenterology
- Nationwide Children’s Hospital
Pediatric Hospital Medicine
- Baylor College of Medicine
Allergy/Immunology
- Penn State Milton S. Hershey Medical Center
Pediatric Critical Care Medicine
- Penn State Milton S. Hershey Medical Center
- University of North Carolina
Pediatric Hematology/Oncology
- Penn State Milton S. Hershey Medical Center
Sleep Medicine
- University of Michigan
Allergy/Immunology
- Penn State Milton S. Hershey Medical Center
Dermatology Residency
- University of Puerto Rico
Pediatric Critical Care Medicine
- University of Virginia
Pediatric Emergency Medicine
- Akron Children’s Hospital
- NYU Langone Health
Pediatric Endocrinology
- Emory University
Pediatric Rheumatology
- Penn State Milton S. Hershey Medical Center
Tour Penn State Health Children’s Hospital
Virtual Tour
Penn State Health
Penn State Health is a multi-hospital health system serving patients and communities across 29 counties of Pennsylvania. Its mission is to improve health through patient care, research, education and community outreach.
In December 2017, the system partnered with Highmark Health to facilitate creation of a value-based, community care network in the region. The shared goal of Highmark and Penn State Health is to ensure patients in the community are within:
- 10 minutes of a Penn State Health primary care provider
- 20 minutes of Penn State Health specialty care
- 30 minutes of a Penn State Health acute care facility
Learn more about Penn State Health

Penn State Health Children’s Hospital (left), Penn State Health Milton S. Hershey Medical Center (center) and Penn State Cancer Institute (right)
Penn State Health Milton S. Hershey Medical Center
500 University Dr., Hershey, Pa., 17033 (Derry Township, Dauphin County)
- The health system’s 647-bed flagship teaching and research hospital
- The only medical facility in Pennsylvania accredited as both an adult and a pediatric Level I (highest-level) trauma center
- Dedicated surgical, neuroscience, cardiovascular, trauma and medical intensive care units
- Accredited Life Lion critical-care transport providing more than 1,100 helicopter and approximately 750 ground ambulance transports per year
- More than 1,300 faculty members and more than 650 residents and fellows
- Approximately 29,000 admissions, 73,000 emergency department visits, 1.1 million outpatient visits and 33,000 surgical procedures annually
- Designated as a Magnet hospital since 2007
Learn more about Milton S. Hershey Medical Center
Penn State Health Children’s Hospital
600 University Dr., Hershey, Pa. 17033 (Derry Township, Dauphin County)
- An eight-story, 263,000-square-foot-facility built in 2013 and expanded in 2020
- 146 licensed pediatric beds, 18 acute care beds and a 56-bed neonatal intensive care unit
- Level IV (highest-level) neonatal intensive care unit
- Level I quaternary (highest-level) pediatric intensive care unit
- Level I (highest-level) pediatric trauma center designation
- Intermediate care unit
- Dedicated pediatric operating rooms
- More than 150,000 pediatric outpatient visits and approximately 5,000 pediatric patient discharges annually
Welcome to Hershey
More About Hershey
Interested in learning more about living and working in Hershey, Pa.? See details here:
Wellness, including emotional, spiritual, social and physical health, is a crucial component to training and to becoming a professional, compassionate and resilient physician. Self-care is a skill which must be continually practiced and reinforced. Penn State College of Medicine and Penn State Health are committed to addressing wellness among residents and fellows, with multiple resources readily available.
Institutional resources
- Visit BeWell – a health program designed to support Penn State Health employees
- See Penn State College of Medicine wellness resources here
- Employee Health Care Concierge and Case Management Service
- Partners in Medicine
Moving to a new city with your family does not have to be stressful. Residency programs have assisted many significant others with finding employment. There is also a GME-Wide Partners in Medicine (PIM) group that offers networking opportunities as well as various social and community oriented activities. - The Doctors Kienle Center for Humanistic Medicine
- Active and easily accessed Office of Professional Mental Health
Graduate medical education resources
Program Resources
The program knows that residency can be a challenging time in any young physician’s life and so takes wellness seriously. The Pediatric Residency offers the following wellness initiatives:
- PAWS (pediatric administrative and wellness sessions) every other week focusing on the eight dimensions of wellness (physical, emotional, social, intellectual, environmental, spiritual, vocational, and financial)
- Monthly “JEDI (Justice, Equity, Diversity, Inclusion) Council” facilitated by pediatric residents and/or faculty.
- Timely debrief sessions following traumatic events such as codes, traumas or deaths
- Quarterly class wellness nights
- Biannual wellness half-days
- Semiannual residency wellness events
- Yearly class retreats (including three in intern year)
- House staff sessions every 2-4 weeks to discuss and address any resident concerns
- Resident families (assigned shortly after Match Day)
- Resident clubs (e.g., running, hiking, books, TV, board games, etc.)
- Resident-led wellness/social committee
- Resident coaches (assigned upon arrival for intern year)
- Opt-out mental health sessions are coordinated with the Office of Professional Mental Health to offer confidential check-in sessions with the option to continue services, if desired. The residency program identifies optimal meeting times to ensure residents are able to attend.
Resident Retreats






Diversity in Dauphin County, Pa
Residents have the opportunity to work with a diverse patient population within our clinics, which are primarily located in Dauphin County (Hershey and Harrisburg). Demographics of gender, race, ethnicity and socioeconomic status mirrors that of the United States as a whole, according to the 2020 U.S. Census Bureau.
Department of Pediatrics Diversity, Equity and Inclusion Council
The Department of Pediatrics Diversity, Equity and Inclusion (DEI) council is composed of physicians (including residents) and nurses from across the Department of Pediatrics. The council’s mission is to continually improve the inclusivity and equity with which the Penn State College of Medicine Department of Pediatrics provides healthcare, medical training, and advances medical science by:
- Providing pediatric patients and their families with excellent, compassionate, culturally responsive and equitable care.
- Supporting the department in recruiting, hiring and retaining a group of diverse faculty, trainees and staff, while equipping Department members to provide culturally responsive and equitable care.
- Ensuring that scholarly pursuits account for, evaluate and address potential social determinants of health beyond race and ethnicity, and that our research reflects a diverse and representative population.
- Striving to ensure our educational experiences foster and value equity, inclusivity, cultural competency and the needs of a diverse population.
Institutional Resources
Penn State Health and Penn State College of Medicine celebrate, embrace and support the diversity of all patients, faculty, staff, students and trainees.
Office for Diversity, Equity and Inclusion
In keeping with this, Penn State Health has an active Office for Diversity, Equity and Inclusion with various programs, networks and resource groups, including:
- Talks and lectures on diversity, equity and inclusion through the Inclusion Academy
- Regular events on topics such as eradicating racism and creating a culture of inclusiveness
- Many Business Employee Resource Groups (BERGs), including:
- Disability Business Employee Resource Group
- Interfaith Business Employee Resource Group
- LGBTQ+ Business Employee Resource Group
- Military and Veterans Business Employee Resource Group
- Multicultural Business Employee Resource Group
- NextGen Business Employee Resource Group
Learn more about the Penn State Health Office for Diversity, Equity and Inclusion
Learn more about the College of Medicine’s Office for Diversity, Equity and Belonging
Office for Culturally Responsive Health Care Education
The vision at Penn State College of Medicine and Penn State Health is to equip learners with the knowledge, skills and attitudes they will need to provide culturally excellent health care and research for an increasingly diverse U.S. population. The Office for Culturally Responsive Health Care Education was formed to help meet that goal.
Learn more about the Office for Culturally Responsive Health Care Education
Office for a Respectful Learning Environment
In addition, the institution does not tolerate discrimination, biases, microaggression, harassment or learner mistreatment of any kind, and any concerns are immediately addressed by the Office for a Respectful Learning Environment.
Learn more about the Office for a Respectful Learning Environment
Network of Under-represented Residents and Fellows
The Network of Under-represented Residents and Fellows (NURF) is a group of diverse residents and fellows representing all specialties. NURF’s goal is to promote cultural diversity in the residency programs through community involvement, mentorship with diverse faculty, professional networking and support for the recruitment of diverse medical students into the residency programs.
NURF is sponsored by the Penn State College of Medicine Graduate Medical Education Office and the Penn State Health Office for Diversity, Equity and Inclusion.
Learn more information about NURF
Anti-Bias Policy
Penn State Health and Penn State College of Medicine celebrate, embrace and support the diversity of all patients, faculty, staff, students and trainees. Beginning in May 2017, Penn State Health’s Patient’s Rights and Responsibility Policy was updated to include a section stating that patients cannot decline the care of a provider based on the provider’s race, religion, gender, age or sexual orientation. Penn State Health became one of the first health care systems nationwide to establish an official anti-bias policy that protects providers when such cases arise.

Program Resources
The pediatric residency program also hosts a monthly “JEDI (Justice, Equity, Diversity, Inclusion) Council” facilitated by pediatric residents and/or faculty. Past topics include gender bias, disability and race in medicine.
Resident Perks
- Annual book money allowance
- Residency pays for copies of Harriet Lane and Bright Futures Pocket Guide
- Departmental travel grants up to $2,000 for presenting research at conferences (including free poster production)
- “Meal Money” to be used at hospital cafeterias or Starbucks
- Program additionally provides lunch twice per week
- Stocked resident fridge (free meals, snacks and drinks at night)
- Free American Academy of Pediatrics (AAP) membership providing monthly print journals (Pediatrics and Pediatrics in Review) as well as Board Review Questions (PREP)
- Free board preparation question banks and teaching materials.
- Free certifications and updates of BLS, PALS, NRP and ATLS.
- Free on-site parking
- Retreats and wellness events paid for by residency
- Yearly lunch with the Chair of Pediatrics
For medical school students
Penn State Health Children’s Hospital offers four acting internships and multiple other subspecialty electives as fourth year medical student experiences. Medical students interested in an away rotation at Penn State Health Children’s Hospital should view visiting student eligibility and application requirements here. General questions about the application process and logistics should be directed to smiller29@pennstatehealth.psu.edu.
Any student applying for an away rotation because of a strong interest in completing their pediatric residency training at Penn State Health Children’s Hospital are strongly encouraged to email program directors japrile1@pennstatehealth.psu.edu or ashedlock@pennstatehealth.psu.edu.
Visiting Residents
All information and the application for visiting residents can be found here.
Observerships, Shadowing, Internships and Externships
The pediatric residency program does not schedule or coordinate shadowing, externship, research internship or observership opportunities. This is coordinated separately by the Penn State College of Medicine and Penn State Health. Inquiries for student placement or shadows can be directed to Ashley Gunkle at agunkle@pennstatehealth.psu.edu or to the Chief Learning Officer and team at affiliationagreements@pennstatehealth.psu.edu.
For residency related matters, please call 717-531-5685.
Mailing Address
Penn State Health Children’s Hospital
Pediatric Residency
500 University Dr., Mail Code H085
P.O Box 850
Hershey, PA 17033
Curriculum Details
The Pediatric Residency curriculum is designed around the individual educational needs of residents, rather than being dictated by the needs of the hospital. The residency has purposely stayed away from “tracks” in the design of its curriculum as the program is large enough to offer virtually every possible rotation, but also small enough to design individualized programs without constraining residents into tracks. In essence, this allows each resident to form their own personalized “track”.
As such, there is an appropriate balance of outpatient and inpatient experiences, and the program provides an extensive individualized curriculum that goes far beyond the minimum requirements of the ACGME.
The program’s goal is that each resident graduates as a competent outpatient and inpatient general pediatrician who is also well-prepared for the next step in their career. This balanced approach is reflected in the fact that approximately half of recent graduates went into either primary care or hospital medicine, while the other half pursued fellowship training.
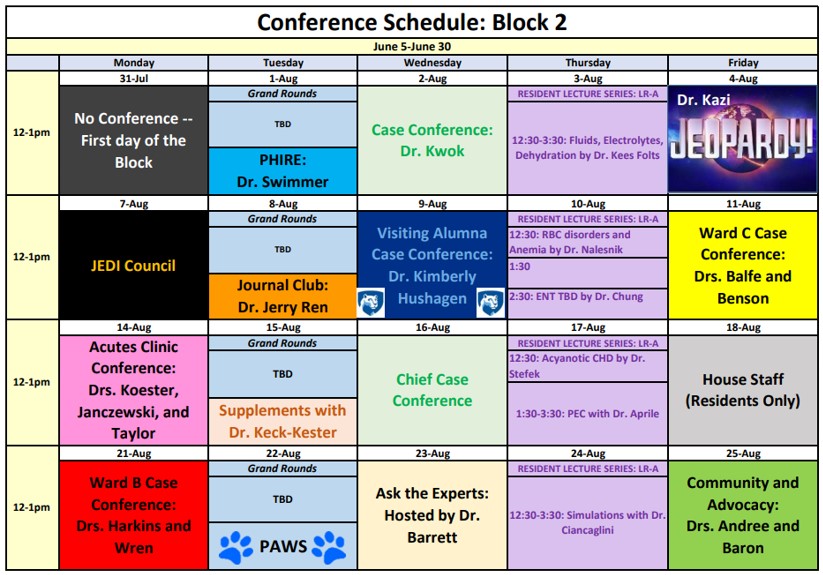
In addition to clinical rotations, the resident educational curriculum includes daily noon conferences, a weekly protected academic half-day, weekly departmental Grand Rounds, a Residents as Educators lecture series and a Diversity, Equity and Inclusion lecture series.
The following topics are longitudinally represented throughout the residency educational experience:
- Care of deteriorating patient – monthly simulation sessions and monthly mock codes
- Career development
- Diversity, equity and inclusion
- Health systems science
- Health care disparities and advocacy – monthly topics and longitudinal three-year class project
- Moral distress/trauma debriefings
- Quality improvement
- Patient safety – resident-led quarterly morbidity and mortality conferences
- Primary care anticipatory guidance topics – monthly “ask the expert” and continuity clinic curriculum
- Residents as educators
- Scientific and evidence-based principles – monthly journal club
- Wellness – bimonthly pediatric administrative and wellness sessions (PAWS)
The longitudinal primary care continuity clinic experience is special in many ways:
- Each resident is paired with one outpatient preceptor for the entire three-year residency, allowing for many personalized mentorship and feedback opportunities.
- Each resident will have the choice of five different continuity site locations, ranging from a large academic hospital-based clinic to a more urban/underserved clinic to a more suburban/rural practice setting. There are private clinic opportunities as well.
In addition, there is a monthly continuity clinic curriculum with rotating primary care core topics to be discussed in small-group settings during clinic sessions.
Highlights
The first-year curriculum purposefully integrates numerous outpatient and elective experiences to balance the inpatient experience.
Adolescent medicine: The primary clinical site for this four-week rotation is the Milton Hershey School, a large, cost-free, private boarding school for children from families of low income and limited resources. The rotation also includes time in clinics for adolescent gynecology, addiction medicine and eating disorders.
Community and advocacy: This four-week rotation includes clinical time at two pediatric clinics in Harrisburg, Pa., committed to serving children in under-resourced areas as well as in outpatient and inpatient child abuse settings. It also features a wide-variety of non-clinical experiences that expose residents to many community resources that can assist their patients. These experiences include spending time with:
- Lawmakers and lobbyists at the state capitol
- Penn State Law, working with a children’s advocacy program
- Children and Youth Services
- Home nursing
- Lactation services
- Pediatric rehabilitation/care coordination
- Early intervention
- Opioid clinic
- Pediatric dentistry
Also offered is dedicated time and training on quality and improvement methods and how to complete a needs assessment in order to implement community-based changes benefiting the children of central Pennsylvania and beyond. This serves as the starting point for the class advocacy/health care disparity project.
First-Year Rotations
The first-year rotations are:
Inpatient
- Hospitalist team – six to eight weeks
- Inpatient gastrointestinal/cardiology/nephrology team – two to four weeks
- Inpatient pulmonology team – two to four weeks
- Neonatal ICU – four weeks
- Newborn nursery – two weeks
- Night team – six weeks (divided into three rotations)
Outpatient
- Acute clinic – four weeks
- Adolescent medicine – four weeks
- Community and advocacy – four weeks
- Emergency medicine – four weeks
- Individualized curriculum/electives – six weeks
Other
- Longitudinal continuity clinic
- Vacation – four weeks
Highlights
The second year continues to offer a balanced curriculum (along with increased time for electives as part of the individualized curriculum) while building senior resident leadership skills and increasing comfort with more severely ill patients.
Developmental/behavioral pediatrics: This rotation includes time in a broadly focused developmental-behavioral clinic, plus time focused on:
- Sleep disorders
- Speech therapy
- Audiology
- Palliative care
- ADHD
- Feeding disorders
- PKU
- Tic disorders
- Autism
- Behavior modification
- Educational evaluation
- Brain injury
Independent Hospitalist Experience: The rotation is a unique opportunity to mimic the community hospitalist experience where a resident is given a panel of inpatient general pediatrics patients to triage and manage independently throughout the day under the direct supervision of a hospitalist physician. There are no formal teaching rounds but many informal opportunities for one-on-one attending instruction on triaging, coordinating care, admitting, discharging, and fielding outside hospital phone calls for direct admissions.
ED consult: This rotation is an opportunity that allows pediatric residents to be on the front lines of pediatric assessment, evaluation, treatment and care. When children in the Emergency Department represent a challenging case or will potentially need to be admitted, the ED consult resident evaluates and triages the patient, then works one-on-one with the pediatric hospitalist, pediatric intensivist and many of the pediatric subspecialists to formulate an appropriate plan of care, including:
- Admission criteria and decisions on bed placement and appropriate level of care
- Coordination with the outpatient transitional care clinic, especially for “diagnostic dilemmas” that don’t meet admission criteria but require continued workup and evaluation
- Discharge criteria and needed follow-up
Second-year rotations
The second-year rotations are:
Inpatient
- Inpatient gastrointestinal/cardiology/nephrology team senior – two weeks
- Inpatient hematology/oncology/stem-cell transplant team – four weeks
- Inpatient pulmonology team senior – two weeks
- Independent Hospitalist Experience – two weeks
- Neonatal ICU – four weeks
- Night team senior – six weeks (divided into three rotations)
- Pediatric ICU – four weeks
Outpatient
- Daytime ED consults – two weeks
- Developmental/behavioral pediatrics – four weeks
- Emergency medicine – four weeks
- Individualized curriculum/electives – 14 weeks
Other
- Longitudinal continuity clinic
- Vacation – four weeks
Highlights
The third year purposefully allows for significant flexibility for residents to structure their individualized curriculum to best suit their needs before starting a first job or fellowship. The curriculum focuses on leadership opportunities and on career development. Although it appears as if most rotations are in the inpatient setting, most residents will spend the majority of individualized elective time in the outpatient setting.
School-based community health and advocacy: All residents spend two weeks at the local Milton Hershey School, which is a cost-free private boarding school started by Milton and Catherine Hershey to service children with family hardships. This rotation provides independent outpatient clinical experience with the opportunity to mentor children, teach school-wide health seminars and influence school health policies.
Resource resident: Implemented as a “flex opportunity” to promote wellness of individual residents (providing weekdays off) and the residency as a whole (filling in clinical coverage gaps and providing an extra resident to help when needed).
Selectives: Allow residents to perfect their senior resident skills on the services of their choice, including inpatient gastrointestinal/cardiology/nephrology team, inpatient hematology/oncology/stem-cell transplant team, inpatient pulmonology team, newborn nursery team, pediatric ICU team or as emergency department consult resident.
Third-Year Rotations
The third-year rotations are:
Inpatient
- Hospitalist team senior – four weeks
- Newborn nursery team senior – two weeks
- Pediatric ICU – four weeks
- Resource resident – two weeks
- Selectives – eight weeks
Residents also spend an additional eight weeks perfecting their senior resident skills on the services of their choice, including inpatient gastrointestinal/cardiology/nephrology team, inpatient hematology/oncology/stem-cell transplant team, inpatient pulmonology team, newborn nursery team, pediatric ICU team or as emergency department consult resident.
Outpatient
- Acute clinic team senior – four weeks
- Overnight ED consult – two weeks
- School-based community health and advocacy (Milton Hershey School) – two weeks
- Individualized curriculum/electives – 20 weeks
Other
- Longitudinal continuity clinic
- Vacation – four weeks
The ACGME requires pediatric residencies to provide 24 weeks of individualized education. The Pediatric Residency at Penn State Health Children’s Hospital places the needs of residents and their interests over the needs of the hospital and offers a total of 10 blocks (40 weeks) of individualized education, many of which can be broken up into two-week experiences.
In addition, variable scheduling on inpatient rotations in the third year (the “selectives”) creates another eight weeks of somewhat individualized time.
Punit Jhaveri, MD, serves as the director of individualized education. In this role, he is given time away from his clinical responsibilities for the specific purpose of helping residents choose rotations for the following year.
The program can individualize certain rotations to coincide with the resident’s career goals. Note that the residency has purposely stayed away from “tracks” in the design of its curriculum. The program is large enough to offer virtually every possible rotation, but also small enough to design individualized programs without needing to rely on tracks.
Although there are a few rules to follow regarding the choice of rotations, most residents are simply able to take the desired rotations from this list or create and customize their own elective rotation to meet their individual goals:
- Abuse/neglect
- Acute clinic
- Adolescent medicine
- AHEC underserved medicine
- Allergy/immunology
- Anesthesiology
- Breastfeeding
- Cardiology
- Complex care
- Dermatology
- Eating disorders
- Emergency medicine
- Emergency medicine procedures
- Endocrinology
- Gastroenterology
- Genetics
- Hematology/oncology
- Hospitalist
- Infectious diseases
- Life Lion (Emergency Transport Services)
- Nephrology
- Neurology
- Neurosurgery
- NICU
- Ophthalmology
- Orthopaedic surgery
- Otolaryngology
- Palliative care/hospice
- Pathology
- Pediatric surgery
- PICU
- Pulmonology
- Private practice
- Procedures
- Psychiatry
- Radiology
- Research
- Rehabilitation
- Rheumatology
- Sports medicine
- Urban primary care
- Weight management (obesity) clinic
In the self-managed individualized learning elective (SMILE), residents can take up to four weeks to design their own learning goals and objectives and can even work from home (i.e., reading block).
Based on resident feedback, our program implements a night float rotation system which significantly improves wellness. There are No intern 24-hour calls, No senior 28-hour calls and only about 3 total senior level 24-hour call shifts over the course of the 36-month residency schedule. By resident request, we otherwise mostly utilize a 12 days on/2 days off inpatient schedule to maximize the number of free “golden weekends.”
Resident-led noon conferences occur four days a week, covering interesting clinical cases, primary care topics, journal club, research topics, quality improvement, DEI topics, health care disparities, advocacy, global health, wellness topics and board review. The program also periodically invites residency alumni back to speak in the career development series to share their experiences.
An academic half-day consists of faculty-led didactics and simulation lab experiences on Thursday afternoons, with clinical coverage provided and pagers/phones held. These topics compose the core curriculum, repeating every 18 months, and are based on the board exam specification content outline of the American Board of Pediatrics.
Other educational opportunities include:
- Mock trial malpractice course, in collaboration with Penn State Law
- Residents as Educators lectures and courses (in partnership with the Woodward Center)
- Multifaceted clinical simulation center
- Global health opportunities, including institution-wide affiliation with Ghana
- Diversity, Equity and Inclusion lecture series and Inclusion Academy
- Research elective and mentorship, including the Physician Scientist Training Program
- Free membership for all residents to Med Study (board review questions).
The multifaceted Clinical Simulation Center is a 9,500-square-foot space including some small encounter rooms, three larger bays, skills training areas and rooms for debriefing purposes.
Many educational opportunities are provided here, including a simulation instructor course (resulting in a certificate in simulation education), the Resuscitation Sciences Training Center and a standardized patient program. Along with full-bodied manikins of all ages, there are many types of clinical equipment in order to practice clinical diagnosis and treatment, as well as simulation scenarios such as procedures, surgery and trauma.
The Clinical Simulation Center is staffed for a majority of the day each weekday. The Pediatric Residency incorporates simulation lab didactics during one academic half-day each quarter.
Learn more about the Simulation Center
Pediatrics SIM Curriculum
Situ simulation sessions are focused on improving resident self-efficacy in assessment and stabilization of critically ill children. Sessions are run by chief residents solely for pediatric residents to provide protected educational space for targeted teaching of knowledge and skills.
In conjunction with Penn State College of Medicine, the Pediatric Residency offers many exciting opportunities to further trainees’ development as medical educators:
- Health Systems Science Academy (HSSA)
- One PGY-2 trainee is chosen each year as a Health Systems Science Scholar with protected time to complete the HSSA.
- Woodward Center educator development resources and programs, including:
- Quarterly “Residents as Educators” core lecture series
- Quarterly “Teaching Champion” retreats
- Two-week cross-specialty medical education elective for residents
- Longitudinal “Clinician Educator” medical education pathway
- Woodward Scholars Program
- Opportunity for 100 percent tuition discount for a graduate certificate (12 credits) in adult education from Penn State Harrisburg. Credits can later be applied toward a master’s degree (30 credits).
- EdVenture Conference: the College of Medicine’s annual celebration of teaching and learning.
- PGY-2, James Fisher, DO, presented a poster at the EdVenture annual conference on April 27, 2023: “Improving Pediatric Discharge Summaries Through an Interactive Curriculum”
- The Exceptional Moments in Teaching program highlights outstanding resident and fellow teachers at Penn State Health. Residents from each class are also honored with teaching awards each year at graduation.
Penn State Health and Penn State College of Medicine have nationally recognized investigators with numerous grants and NIH funding in the fields of basic/bench, clinical, translational and health services research.
Through extensive individualized curriculum opportunities, residents have the ability to work alongside these researchers longitudinally and/or during research electives. Residents can schedule as many as 20 weeks of individualized time for research. Those highly interested in a future research career can also consider the Physician-Scientist Training Program to receive a research certificate and be matched with prolific research mentors and periodically meet with other budding clinical scientists to share ideas.
Approximately 50 percent of program residents participate in research during a given academic year. Residents have disseminated their research at the national, regional and local levels. Penn State Health’s Resident/Fellow Research Day is held yearly to showcase accomplishments. The residency program regularly funds resident posters and travel costs (up to $2,000) to present research.
Residents also have the opportunity to participate in numerous quality improvement/patient safety committees as well as complete projects with expert faculty. Lectures on quality improvement and patient safety are given throughout the year, and periodic workshops in quality improvement are offered. All residents develop a QI project under faculty leadership in their PGY-1 Community and Advocacy rotation aimed at reducing health care disparities.
Residents interested in global health have multiple opportunities at Penn State Health and College of Medicine, including international travel electives and virtual self-directed rotations. Residents can travel to Brazil, Croatia, Bosnia-Herzegovina, and Zambia, but our most popular affiliation/elective is the annual trip to Ghana (see details below).
- When: January or February
- Duration: Four weeks
- About the facility: The program takes place with Penn State Health Children’s Hospital’s clinical partner, Eastern Regional Hospital, a 429-bed hospital that serves as the primary care center for the local community and is the referral hospital for 16 district hospitals in the region. It includes a six-bed intensive care unit, lab, CT scan and X-ray. Many specialties are housed here.
- Rotation details: Experiences in NICU, pediatrics floors and pediatric outpatient clinics. The department funds a significant portion of the trip for multiple residents each year, and upon their return, participant experiences are shared during a Grand Rounds presentation.
Photos from Ghana

Pediatric residents Emily Gibbons and Jake Beerel join the team from the General Pediatrics Wards at the Eastern Regional Hospital, Koforidua, Ghana.

Pediatric residents Emily Gibbons and Jake Beerel accompany a nurse administering vitamins and ensuring local children are up to date on vaccines.

Pediatric resident Emily Gibbons working with the NICU team at Eastern Regional Hospital.

Pediatric resident in the NICU at the Eastern Regional Hospital in Koforidua, Ghana.

Pediatric residents exploring the Kakum National Forest.

Pediatric residents join staff at the Community Base Health Planning & Services in Mampong, Ghana

Pediatric resident in the NICU at the Eastern Regional Hospital in Koforidua, Ghana.
Penn State Health Children’s Hospital is situated just 13 miles from Pennsylvania’s capital of Harrisburg and 130 miles from Washington, D.C., providing numerous opportunities for local, state and national advocacy.
- All residents are taught basic principles of social determinants of health and advocacy during their first-year Community and Advocacy four-week rotation.
- Each intern completes a “windshield survey” of the local community to later develop a community-based QI project proposal.
- Residents choose a class-based health care disparity/advocacy project and are provided protected time to work on this project longitudinally to serve the community during residency.
- Class of 2023 Project – Firearm Safety
- Presented at a regional APPD meeting and awarded a $1000 grant.
- Class of 2024 Project – “Residents in Schools”
- Class of 2025 Project – “A Shot To Live” – School-based anaphylaxis recognition and management teaching
- Presented at the National AAP (2022) and PAS (2023) Meetings
- Class of 2023 Project – Firearm Safety
- All residents rotate at a boarding school for disadvantaged children and participate in school-based community health and advocacy for two weeks during the third year.
- Residents facilitate a monthly community and advocacy noon conference.
- The residency program funds all resident memberships to the American Academy of Pediatrics (AAP).
- The program also encourages residents to participate in Advocacy Day in Harrisburg each spring. Residents connect with their peers and meet with PA state legislators to promote policy change.
- The 2023 Advocacy Day focused on juvenile justice reform legislation. Residents met with legislators to advocate for Pennsylvania Senate Bills 167-170, which propose critical reforms to Pennsylvania’s juvenile justice system.
Residents participating in the 2023 PA Advocacy Day at the State Capital in Harrisburg. From left, Natalie Balfe, Melissa McGovern, Talbot Weston, Kristen Sanchez, Christine Tichonevicz.
- The 2023 Advocacy Day focused on juvenile justice reform legislation. Residents met with legislators to advocate for Pennsylvania Senate Bills 167-170, which propose critical reforms to Pennsylvania’s juvenile justice system.
- Milton Hershey “Project Fellowship” Big Sibling Mentorship Program – residency program has “adopted” a student house at the private boarding school to engage in mentorship and social activities.

Penn State Health Pediatrics residents from the Milton S. Hershey Project Fellowship Mentoring Program participated in a Big Sibling event on October 22, 2022, at the local Risser Farm Market. Residents enjoyed time with the young ladies of Moldavia riding hayrides, roasting hotdogs and completing a corn maze.
- Student Home Moldavia holiday event.

Resident volunteers from Project Fellowship participated in a holiday event on Sunday, December 11, 2022, with girls from Student Home Moldavia. All enjoyed an evening of decorating cookies, playing minute-to-win-it games, and a candy cane hunt! There was no shortage of laughs or treats!
- Resident volunteers from Project Fellowship participated in a Tie-Dye project and S’mores event with girls from Student Home Moldavia.

Residents Connor Appelman, Kyle Powers, Kristen Sanchez, Talbot Weston, Virginia Byrd, Morgan Cash, and Leslie Abraham roast marshmallows and make s’mores with girls from Student Home Moldavia.
- Pediatric Residency Advocacy Interest Group – community engagement and legislative advocacy.
- One PGY-2 trainee is chosen each year as the pediatric residency’s:
- AAP Advocacy Delegate (including free travel and registration to the yearly AAP conference)
- Health Systems Science Scholar, to participate in the Health Systems Science Academy
- PA-AHEC Scholars Program: The residency program is partnering with Pennsylvania Area Health Education Center to offer residents the opportunity to participate in the Scholars Program.This is a 2-year customizable elective where residents gain hands-on experience working with underserved, marginalized and rural populations. The program includes 80 hours of didactic training (interactive and online) and 80 hours of clinical and community based experiences.
- Penn State Health is very engaged in community health initiatives, presenting many opportunities for residents, including:
Resident Spotlight
 Former PGY-3 resident Connor Appelman completed a quality improvement project: “Improving Patient Access to Primary Care by Reducing Clinic No-Show Rates.” Current literature demonstrates that clinic no-shows lead to delays in preventative care and poorer chronic disease control. This quality improvement project seeks to identify factors driving patient no-shows, evaluate current interventions and propose new interventions to improve appointment retention.
Former PGY-3 resident Connor Appelman completed a quality improvement project: “Improving Patient Access to Primary Care by Reducing Clinic No-Show Rates.” Current literature demonstrates that clinic no-shows lead to delays in preventative care and poorer chronic disease control. This quality improvement project seeks to identify factors driving patient no-shows, evaluate current interventions and propose new interventions to improve appointment retention.
Resident Honors and Recognitions
Resident Spotlight

Heather Ren, MD, PhD
PGY-2 resident Heather Ren, MD, PhD, has been awarded a $15,000 grant from Resident Research Preceptorship through the Rheumatology Research Foundation. The award is provided by an endowment from Dr. Ephraim P. Engleman for three months of research over the course of one year.
Dr. Ren is doing a research project on dermatomyositis with Havell Marcus, MD/PhD candidate; Amanda Nelson, PhD; Matthew Helm, MD; and Acela Christina Rosado, MD. Dr. Ren is researching whether the cytokine IL-21 and tissue resident memory CD8 T cells may be an important step in the pathogenesis of dermatomyositis disease.
Resident Spotlight
Bryan Cusack, DO
Ramin Beheshti, MD
Former PGY-3 resident Dr. Ramin Beheshti and PGY-3 resident Dr. Bryan Cusack have started a program called “A Shot To Live,” which aims to better prepare school staff to manage and treat anaphylaxis in school settings through in-person training simulations. Children often suffer from anaphylactic reactions at school. In 2014, the Pennsylvania Legislature passed Act 195, which allows trained individuals to administer unassigned epinephrine (UE) in an emergency and for schools to store epinephrine auto injectors. A Shot To Live was created to better ensure early recognition, and timely/safe epinephrine administration in school related anaphylaxis.
The Penn State Pediatrics department has provided $2,000 of travel grant money to support Ramin and Brian’s oral platform presentation on this important initiative at the AAP National Conference in Anaheim, CA in October 2022.
Resident Spotlight
Emily Gibbons, MD
PGY-3 resident Dr. Emily Gibbons has been partnering with the Milton Hershey School establishing a new initiative, Project Fellowship. The purpose of Project Fellowship is to foster a sense of community between Milton Hershey School students and the community. Through generous funding from both Milton Hershey School and Penn State Health Milton S. Hershey Medical Center, residents host fun, community building events throughout the year. Examples of events include an end-of-summer picnic, pumpkin picking/carving, Hershey Bears games, multiple outdoor activities such as hiking, and holiday festivities.
Dr. Gibbons is also piloting a new project, Residents in Schools. The goal of this project is to enhance the program’s outreach by providing engaging and interactive education on health-related topics. Educational topics include nutrition, exercise, safety, oral hygiene, transitions of care for high school students and Teddy Bear Clinics for elementary school students.
Resident Spotlight
Talbot Weston, DO
PGY-2 Resident Talbot Weston has been awarded additional funding for the Residents in Schools program through a Community Relations grant. This grant supports the expansion of the Residents in Schools program to another neighboring school in Harrisburg so that residents can further extend their educational outreach to the community.
Below is a list of individualized opportunities for residents and current residents who participate.
Penn State College of Medicine and Penn State Health Milton S. Hershey Medical Center accept ongoing nominations for the Exceptional Moments in Teaching award.
The award, given monthly by the Office for a Respectful Learning Environment, accepts nominations from College of Medicine students who are invited to submit narratives about faculty members, residents, fellows, nurses or any other educators who challenge them and provide an exceptional learning experience. See more about the award here.
Previous nominees from the Pediatric Residency are listed here. Click the + next to a nominee name to read their nominator’s comments.
The annual Resident/Fellow Research Day is held each year (with exception of during the COVID-19 pandemic) on and around the Penn State Health Milton S. Hershey Medical Center campus.
The intent of the event is to provide an opportunity for residents and fellows to showcase their research accomplishments to their peers in other clinical departments, as well as their colleagues in the basic sciences.
Learn more about Resident/Fellow Research Day here.
Previous presentations from the Pediatric Residency are listed here.
Latest News from Penn State Health Children's Hospital









