Jump to topic
Search
Program Highlights
- Two EMS physician response vehicles
- Hospital-owned and operated air and ground critical care transport teams
- Hospital-based EMS system covering urban and rural areas
- Mass gathering medicine at Penn State University football games at Beaver Stadium (more than 100,000 seats)
- Disaster medicine training with FEMA/USAR resources
- EMS special operations including tactical, search and rescue, fire, and HAZMAT
- Community paramedicine program
- Dedicated Mobile EMS ambulance simulator and access to the Clinical Simulation Center
- Opportunity to earn a master’s degree in public health or homeland security
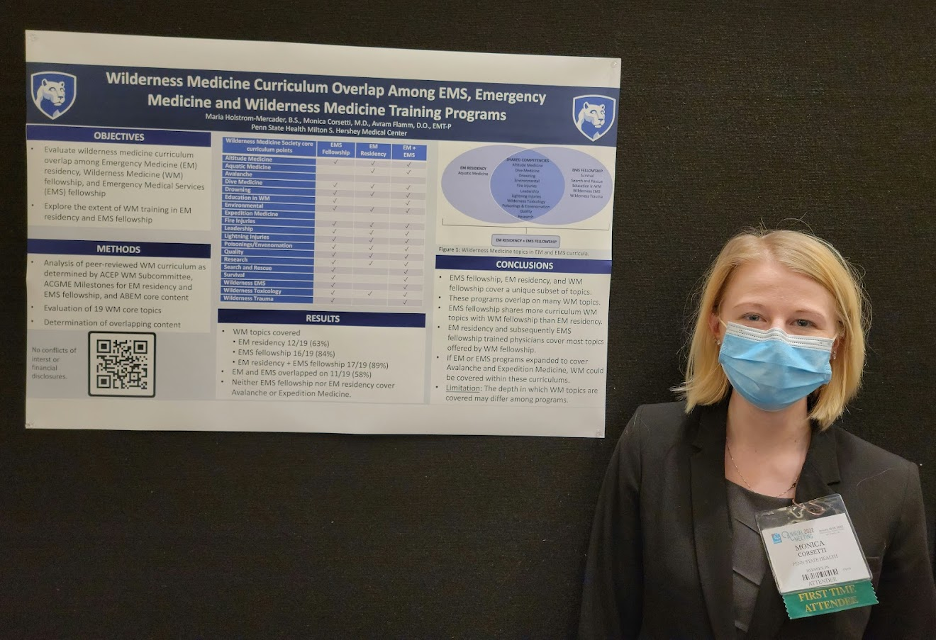
- Diverse research program with successful track record of presentations and publications
- State and national legislative exposure
- International opportunities
Program Details
Penn State Health Milton S. Hershey Medical Center’s Emergency Medical Services Fellowship provides fellows with the experience and training in patient care, operations, research, education and administration needed for the successful practice of prehospital medicine and medical direction of EMS systems.
By the conclusion of their training, fellows will fulfill all ACGME requirements and be exceptionally well prepared to begin working as an EMS physician in any agency. Moreover, the program provides an individualized experience for each fellow with flexibility to pursue personal clinical, professional and scholarly interests. Additional in-depth and expanded experiences can be arranged in all areas listed below.
“One of the qualities of the EMS Fellowship at Penn State Hershey S. Milton Medical Center that I benefited the most from was the fact that the coverage area serviced by LifeLion is so diverse. You might see patients in an urban, suburban and rural environment in one day. The Fellowship is well set up to allow for flexible fellow response.”
– Chris Berry, MD
The program operates two, fully licensed and equipped physician response vehicles, with fellow field response beginning immediately after orientation. The coverage area for 911 response includes most of Dauphin County, and a large portion of Lebanon and Berks counties. Life Lion LLC also covers a large area on the west side of the Susquehanna River.
Fellows work closely with the medical director for ground Life Lion EMS and with the operation’s directors, supervisors and managers. Active participation on a number of committees such as QA/QI and Practice Council is required. Fellows help review charts of new hires and those under disciplinary action and do periodic focused review of chief complaints, procedures or medication use. They also lead monthly total quality management meetings between directors, managers, supervisors and physicians and will perform policy reviews and updates. By the third month, fellows begin to function as medical directors on call.
Rounding out the fellowship experience are additional opportunities in vehicle rescue, fireground operations, and with both the Life Lion Communications Center and the Dauphin County PSAP. Fellows may also choose to attend the FDNY Annual Medical Special Operations Conference or CONTOMS. Practical field experience is complemented by a full series of didactic presentations and by the annual NREMT and NAEMSP Medical Director courses.
The program provides EMS fellows with the knowledge and understanding of air medical and critical care transport (CCT) medicine through extensive air and ground operations. Field experience is complemented by a number of didactic and hands-on training throughout the year. While flying is not compulsory, the fellow can take part in both inter-facility (CCT) and scene call responses by air in one of the few hospital operated HEMS services in the country. Operating out of two bases in central Pennsylvania, the service flies more than 1,000 missions each year.
Fellows take part in a flight physician course early in the fellowship and can then function as a CCT team member for the remainder of the year. They learn to operate vents, pumps and monitors in the confines of the helicopter and if interested help transport these patients including those on ECMO, intra-aortic balloon pumps (IABP), LVAD, neonatal isolates, oscillators and with NO gas. Additional transports occur using ground units. The program offers additional opportunities in critical care unit rotations such as the Heart and vascular ICU, ECMO transport workshop as well as quality improvement, and protocol and policy development for CCT.
There are also currently a number of research opportunities in the field of CCT including pre-hospital ultrasound. Interested fellows are encouraged to join the NAEMSP’s Air Medical Services committee or the Critical Care Airway Task Force and other national committees and attend national conferences on air medical transport.
The principal venues are Beaver Stadium, Giant Center arena and Hersheypark. Fellows provide medical care for Penn State NCAA Division 1 home football games at Beaver Stadium, which seats approximately 106,572 people and is the second largest college football stadium in the United States, eclipsed only by Michigan with 107,601 seats. In addition, some of the games are attended by an additional 100,000 tailgaters.
Fellows can also provide medical coverage for Hersheypark Stadium, a popular summer concert venue that attracts major artists, while the Giant Center hosts events year round and is home to the Hershey Bears (American Hockey League) games. There are also additional opportunities including the Hershey Half-Marathon, local festivals and football games, and in election years various political events including presidential visits and motorcades.
One current faculty member and several EMS providers are members of the FEMA Urban Search and Rescue Pennsylvania Task Force One and were deployed to Florida for the condo collapse in 2021. Fellows participate in hospital disaster committee meetings, as well as in hospital, EMS, airport, stadium and Hersheypark mass casualty drills. They also participate in a regional EMS fellow USAR training day, and conduct a full-scale functional exercise in compliance with federal, state and local requirements. Fellows may, and often do, choose to attend the FDNY Annual Medical Special Operations Conference.
The program’s disaster medicine and emergency preparedness training curriculum is intended to provide EMS fellows with a basic working knowledge in this field and offer them the ability to become leaders in their organizations in emergency preparedness and disaster medicine and participate in USAR on a regional and national level through local and FEMA task force work. Fellows may also join the NAEMSP’s Emergency preparedness committee or similar national committee, and may choose to attend disaster conferences.
The program offers experience in community paramedicine (also known as mobile integrated healthcare) and public health. Life Lion has a very unique hospital-based community paramedicine program that was developed in 2017 with a goal of reducing all-cause 30-day readmission rates for patients discharged from the hospital. Beginning with CHF patients, the program rapidly expanded to address other disease processes that include stroke, ventricular assist devices, diabetes and COPD. Due to the success of this program, it continues to expand both in employees and geographically. Fellows are able to work closely with the medical director and the community paramedics and perform home visits while assisting with quality assurance and policy review.
Additional opportunities are offered in local, regional and national conferences, and serving on national committees. There are also opportunities in research with this new and expanding area of EMS. Exposure to public health is provided by didactics, legislative activities and potentially enhanced by international experiences. Fellows can also choose to pursue a graduate degree through Penn State.
The EMS division is committed to advancing knowledge in the field of prehospital care. Several faculty members sit on editorial boards of journals in the field or serve as journal reviewers. Dr. Jeffrey Lubin, the previous fellowship director, is the Department of Emergency Medicine’s Vice Chair for Research and continues to be active as an EMS physician. There are multiple studies ongoing at any given time, and research is presented at regional, national and international conferences, sometimes by the fellows themselves.
Fellows will be, at minimum, expected to complete the scholarly work required by the ACGME for graduation, and all recent fellows have presented their work at the NAEMSP Annual Meeting during their fellowship. They will have the opportunity to join and contribute to the work of the NAEMSP research committee. The university and College of Medicine have ample resources in Translational Science, Qualitative and Mixed Methods Research, grant assistance and more.
Medical students, emergency medicine residents and the EMS fellows take advantage of the wilderness areas surrounding Hershey for a variety of outdoor training opportunities throughout the year. Some of the program’s faculty are Fellows of the Academy of Wilderness Medicine (FAWM). Together with the support of several EMS providers interested in wilderness medicine, they provide a number of opportunities for hands-on training in the wild. The program’s EMS curriculum also has a wide range of wilderness medicine related topics incorporated into didactics, and the program supports fellow participation in regional wilderness medicine conferences and research related to wilderness medicine if they so desire. In fact, it is possible to work on completing the Wilderness Medical Society requirements for Fellow of the Academy of Wilderness Medicine.
Education of EMS providers is a crucial role for any medical director or EMS physician. Principles of adult education are covered in didactics, and the fellow will learn to teach with simulation. Fellows can take the week-long “Teaching with Simulation: An instructor Course Certificate Program” offered several times a year by the medical center. The college of medicine also has a large simulation center and Life Lion has a mobile simulation ambulance. Fellows will instruct EMT students and assist with EMS continuing education for all levels of providers including the CCT nurses. Fellows will give several grand rounds throughout the year. As attendings in the emergency department, the fellows are also involved in teaching medical students and emergency medicine residents
Life Lion EMS supports the Dauphin County Crisis Response Team (CRT) providing tactical paramedics for on-scene medical support. Fellows regularly train with the team and help provide them with continuing medical education. Once vetted, fellows can join them on call outs if they desire.
Dr. Francis Mencl has an interest and experience in international emergency medicine and EMS and is frequently an invited speaker at international conferences and events. He participates regularly in the Rallye Rejviz, an international EMS/ambulance competition held yearly in the Czech Republic in Europe. Fellows can attend and participate as judges or competitors. While there, they also visit EMS in Prague, and may go to Vienna, Budapest or Amsterdam. Other opportunities elsewhere in Europe, the Middle East, Asia and South America can be arranged.
Fellows work closely with the Life Lion medical directors and administration in the day-to-day operations while taking part in regular briefings and business meetings. Harrisburg, Pennsylvania’s state capitol, is a 25-minute drive from Hershey, and Washington, DC, is two and a half hours away, making it easy to interact with legislators and gain direct political experience. Fellows attend ACEP’s annual Leadership and Advocacy Conference in May and gain valuable experience on how legislation works and government functions. In addition, they participate in regular meetings of the Emergency Health Services Federation, a regional EMS council for the Pennsylvania Department of Health.
Learn More about the Fellowship
Fellows will gain clinical experience in various models of EMS services supplying pre-hospital care in the local region. These services include hospital-based, fire-based, military, volunteer, critical-care ground and air transport and blended career and volunteer services that are in urban, suburban and rural areas of southcentral Pennsylvania. Program faculty provide medical direction to all of these service models. In addition, fellows will be involved in education and administrative components of these services.
The primary prehospital services with which fellows work include Life Lion EMS and Critical Care Transport.
Clinical resources include a dedicated EMS physician field-response vehicle certified by Pennsylvania as an Advanced Life Support quick-response vehicle. It is equipped with emergency lights/sirens as well as an augmented supply of advanced life support medical equipment and can be used independently for field response by the fellows after adequate training and experience are obtained.
Fellows also provide direct patient care as flight physicians during both on-scene and inter-facility transports. In addition, they provide on-scene medical control at mass gathering medicine events, such as home football games at Penn State’s Beaver Stadium (typical attendance greater than 100,000, with more than 30 EMS crews activated for the event) and other large events, such as concerts at Hersheypark Stadium. These clinical in-field experiences are provided longitudinally over 12 months.
In addition to a robust didactic and hands-on curriculum, fellows gain administrative experience by attending regional and state meetings with the Medical Advisory Committee of the Emergency Health Services Federation (the regional EMS council for southcentral Pennsylvania), the Pennsylvania Emergency Health Services Council and other local EMS councils.
Fellowship didactics take place on Thursday mornings and average 4 hours. This allows for breaks for holidays and study days while still easily meeting the ACGME requirement. Previous fellows come back on a regular basis to help instruct and bring with them valuable experiences and real life lessons learned while building their CV and developing themselves as faculty. Coupled with the large number of expert fellowship and residency faculty, the fellows receive plenty of education. Pediatric topics are taught by our PEM (pediatric emergency medicine) specialists from the Penn State Health Milton S. Hershey Medical Center, while NICU faculty assist with instruction for specialized neonatal transport. Faculty from the Heart and Vascular Institute assist with ECMO and LVAD training. EMS directors and managers also educate fellows on the business of EMS. Simulation plays a major role in many sessions. Complementing the didactic sessions are the NREMT and NAEMSP Medical Directors course that the fellows take every year. The program does joint didactic sessions with other fellowships on a monthly basis, allowing for exposure to additional EMS faculty and fellows.
The fellows work six, 8-hour shifts in the Penn State Health Milton S. Hershey Medical Center Emergency Department as attending faculty and participate in the education of residents in the Emergency Department, in conference and in EMS field experiences.
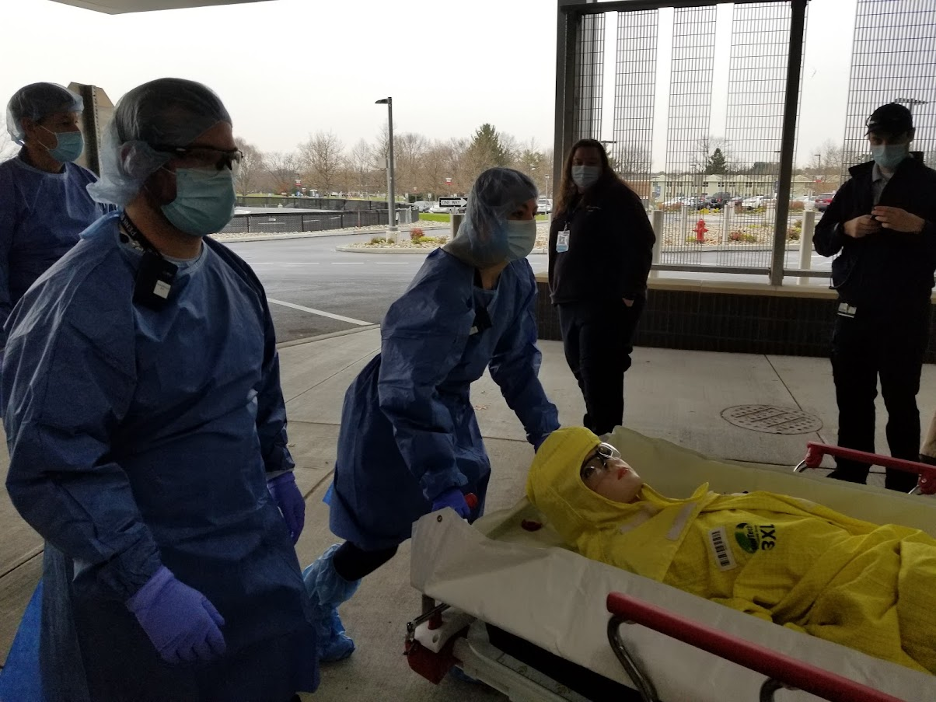
Students in the Emergency Medical Services Fellowship at Penn State Health Milton S. Hershey Medical Center participate in a variety of experiences. Experience in disaster management is integrated into the fellowship curriculum, and a number of mock/drill exercises, some of which are pictured here, are included.
Note: Some photos were taken in 2019 and earlier, before COVID-19 masking requirements were in place.











Eligibility
Candidates must be:
- Board-eligible or board-certified in Emergency Medicine
- Eligible for a Pennsylvania medical training license
All applicants must be graduates of an ACGME-accredited emergency medicine residency prior to beginning the fellowship.
Required Supporting Documents
The following documents should be submitted through the form found below:
- Curriculum vitae
- Letter of interest
- Three letters of recommendation (one from the program director and at least one from an EMS medical director or a practicing EMS Physician)
Submit supporting documents here
Interview Process
Thank you for your interest in our program. Interviews will be held virtually for the 2024-2025 interview season.
Interview dates for 2024 will be:
- Thursday, Sept. 5
- Thursday, Sept. 12
- Thursday, Sept. 19
- Thursday, Sept. 26
The program will be hosting an in-person Second Look Event on Thursday, Oct. 10.
All interviews are by invitation only and applicants will receive further communication via email from EMSFellowship@pennstatehealth.psu.edu.
Important Dates
- Sept. 19, 2024: Application deadline
- Oct. 16, 2024: Rank list deadline
- Oct. 30, 2024: Match results released
Virtual Tour
Penn State Health
Penn State Health is a multi-hospital health system serving patients and communities across 29 counties of Pennsylvania. Its mission is to improve health through patient care, research, education and community outreach.
In December 2017, the system partnered with Highmark Health to facilitate creation of a value-based, community care network in the region. The shared goal of Highmark and Penn State Health is to ensure patients in the community are within:
- 10 minutes of a Penn State Health primary care provider
- 20 minutes of Penn State Health specialty care
- 30 minutes of a Penn State Health acute care facility
Learn more about Penn State Health

Penn State Health Children’s Hospital (left), Penn State Health Milton S. Hershey Medical Center (center) and Penn State Cancer Institute (right)
Penn State Health Milton S. Hershey Medical Center
500 University Dr., Hershey, Pa., 17033 (Derry Township, Dauphin County)
- The health system’s 647-bed flagship teaching and research hospital
- The only medical facility in Pennsylvania accredited as both an adult and a pediatric Level I (highest-level) trauma center
- Dedicated surgical, neuroscience, cardiovascular, trauma and medical intensive care units
- Accredited Life Lion critical-care transport providing more than 1,100 helicopter and approximately 750 ground ambulance transports per year
- More than 1,300 faculty members and more than 650 residents and fellows
- Approximately 29,000 admissions, 73,000 emergency department visits, 1.1 million outpatient visits and 33,000 surgical procedures annually
- Designated as a Magnet hospital since 2007
Learn more about Milton S. Hershey Medical Center
Penn State Health Children’s Hospital
600 University Dr., Hershey, Pa. 17033 (Derry Township, Dauphin County)
- An eight-story, 263,000-square-foot-facility built in 2013 and expanded in 2020
- 160 licensed pediatric beds, 26-bed pediatric intensive care unit and a 56-bed neonatal intensive care unit
- Level IV (highest-level) neonatal intensive care unit
- Level I quaternary (highest-level) pediatric intensive care unit
- Level I (highest-level) pediatric trauma center designation
- Intermediate care unit
- Dedicated pediatric operating rooms
- More than 150,000 pediatric outpatient visits, 20,000 pediatric emergency room visits, and approximately 5,000 pediatric patient discharges annually
Welcome to Hershey
More About Hershey
Interested in learning more about living and working in Hershey, Pa.? See details here:
Wellness, including emotional, spiritual, social and physical health, is a crucial component to training and to becoming a professional, compassionate and resilient physician. Self-care is a skill which must be continually practiced and reinforced. Penn State College of Medicine and Penn State Health are committed to addressing wellness among residents and fellows, with multiple resources readily available.
Institutional resources
- Visit BeWell – a health program designed to support Penn State Health employees
- See Penn State College of Medicine wellness resources here
- Employee Health Care Concierge and Case Management Service
- Partners in Medicine
Moving to a new city with your family does not have to be stressful. Residency programs have assisted many significant others with finding employment. There is also a GME-Wide Partners in Medicine (PIM) group that offers networking opportunities as well as various social and community oriented activities. - The Doctors Kienle Center for Humanistic Medicine
- Active and easily accessed Office of Professional Mental Health
Graduate medical education resources
Institutional Resources
Penn State Health and Penn State College of Medicine celebrate, embrace and support the diversity of all patients, faculty, staff, students and trainees.
Office for Diversity, Equity and Inclusion
In keeping with this, Penn State Health has an active Office for Diversity, Equity and Inclusion with various programs, networks and resource groups, including:
- Talks and lectures on diversity, equity and inclusion through the Inclusion Academy
- Regular events on topics such as eradicating racism and creating a culture of inclusiveness
- Many Business Employee Resource Groups (BERGs), including:
- Disability Business Employee Resource Group
- Interfaith Business Employee Resource Group
- LGBTQ+ Business Employee Resource Group
- Military and Veterans Business Employee Resource Group
- Multicultural Business Employee Resource Group
- NextGen Business Employee Resource Group
- Black Physician Professional Staff Association – Resource Group
- Hispanic Professional Association
- Asian Physician and Professional Staff Association
- International Workforce Inclusion
Learn more about the Penn State Health Office for Diversity, Equity and Inclusion
Learn more about the College of Medicine’s Office for Diversity, Equity and Belonging
Office for Culturally Responsive Health Care Education
The vision at Penn State College of Medicine and Penn State Health is to equip learners with the knowledge, skills and attitudes they will need to provide culturally excellent health care and research for an increasingly diverse U.S. population. The Office for Culturally Responsive Health Care Education was formed to help meet that goal.
Learn more about the Office for Culturally Responsive Health Care Education
Office for a Respectful Learning Environment
In addition, the institution does not tolerate discrimination, biases, microaggression, harassment or learner mistreatment of any kind, and any concerns are immediately addressed by the Office for a Respectful Learning Environment.
Learn more about the Office for a Respectful Learning Environment
Network of Under-represented Residents and Fellows
The Network of Under-represented Residents and Fellows (NURF) is a group of diverse residents and fellows representing all specialties. NURF’s goal is to promote cultural diversity in the residency programs through community involvement, mentorship with diverse faculty, professional networking and support for the recruitment of diverse medical students into the residency programs.
NURF is sponsored by the Penn State College of Medicine Graduate Medical Education Office and the Penn State Health Office for Diversity, Equity and Inclusion.
Mailing Address
Department of Emergency Medicine
EMS Fellowship
Penn State Health Milton S. Hershey Medical Center
500 University Dr.
P.O. Box 850
Hershey, PA 17033-0850
General Contact Information
Phone: 717-531-4604
Fax: 717-531-4441
Latest News from Emergency Medicine





