Jump to topic
Program DetailsLearn More About the FellowshipCurriculum DetailsLatest News from PathologySearch
Program Details
The Hematopathology Fellowship will provide broad exposure to all aspects of the laboratory evaluation of benign and malignant hematolymphoid disorders including automated laboratory testing, coagulation, morphology, immunophenotyping, molecular and cytogenetic methods. The successful fellow will achieve a solid base of competencies to pursue an academic or private practice career.
Penn State Health Milton S. Hershey Medical Center is a 491-bed tertiary-care facility associated with Penn State Cancer Institute, Penn State Children’s Hospital and Penn State College of Medicine. This provides abundant clinical and research material related to benign and malignant, adult and pediatric hematolymphoid diseases including an active bone marrow transplantation program. The hematopathology service also provides consultative services to extramural pathologists and oncologists.
Every year, the hematology laboratories handle more than 1,200 comprehensive bone marrow evaluations; 2,300 flow cytometry interpretations; 600 lymph node, spleen and extranodal tissue samples; 700 peripheral blood smear reviews; 600 hemoglobin evaluations; and 600 coagulation evaluations.
The Molecular Diagnostics Laboratory provides more than 1,000 tests with interpretations to supplement the hematopathology service. The fellow will have dedicated exposure to cytogenetic and FISH techniques related to hematopathology at Quest Diagnostics Nichols Institute in Chantilly, Virginia.
The fellow will participate in research and teaching activities with mentoring from the faculty. Clinically-oriented research opportunities are available with the faculty in the Division of Clinical Pathology and the Division of Anatomic Pathology, and more basic science experiences are available in collaboration with faculty in the Division of Experimental Pathology.
Learn More About the Fellowship
General Application Information
To apply, submit the information listed here via email to esmith31@pennstatehealth.psu.edu.
A complete application will include:
- CAP Standardized Pathology Fellowship Application (found under “Fellowship Resources” at this link)
- Cover letter with personal statement
- Curriculum vitae
- Copy of USMLE test scores (or equivalent)
- Letter of recommendation and verification of training from current/most recent program director
- Two to three additional letters of recommendation
Letters of recommendation may be emailed directly by the references.
Application Requirements
- MD, DO or foreign equivalent with ECFMG certification
- Board-certified or eligible in anatomic and/or clinical pathology from the ABP, or a primary certificate plus a subspecialty certificate in hematology from another member medical specialty board of the ABMS
- Eligible for Pennsylvania medical license
- U.S. citizen, green card holder or J-1 visa holder
Virtual Tour
Penn State Health
Penn State Health is an integrated academic health system serving patients and communities across 15 counties in central Pennsylvania. It employs more than 20,900 people systemwide.
The system includes Penn State Health Milton S. Hershey Medical Center, Penn State Health Children’s Hospital and Penn State Cancer Institute based in Hershey, Pa.; Penn State Health Hampden Medical Center in Enola, Pa.; Penn State Health Holy Spirit Medical Center in Camp Hill, Pa.; Penn State Health Lancaster Medical Center in Lancaster, Pa.; Penn State Health St. Joseph Medical Center in Reading, Pa.; Pennsylvania Psychiatric Institute, a specialty provider of inpatient and outpatient behavioral health services, in Harrisburg, Pa.; and 2,417 physicians and direct care providers at 225 outpatient practices. Additionally, the system jointly operates various healthcare providers, including Penn State Health Rehabilitation Hospital, Hershey Outpatient Surgery Center and Hershey Endoscopy Center.
In 2017, Penn State Health partnered with Highmark Health to facilitate creation of a value-based, community care network in the region.
Penn State Health shares an integrated strategic plan and operations with Penn State College of Medicine, the University’s medical school. With campuses in State College and Hershey, Pa., the College of Medicine boasts a portfolio of more than $150 million in funded research and more than 1,700 students and trainees in medicine, nursing, other health professions and biomedical research.
Learn more about Penn State Health

Penn State Health Children’s Hospital (left), Penn State Health Milton S. Hershey Medical Center (center) and Penn State Cancer Institute (right)
Penn State Health Milton S. Hershey Medical Center
500 University Dr., Hershey, Pa., 17033 (Derry Township, Dauphin County)
- The health system’s 611-bed flagship teaching and research hospital
- The only medical facility in Pennsylvania accredited as both an adult and a pediatric Level I (highest-level) trauma center
- Dedicated surgical, neuroscience, cardiovascular, trauma and medical intensive care units
- Accredited Life Lion critical-care transport providing more than 1,100 helicopter and approximately 750 ground ambulance transports per year
- More than 1,300 faculty members and more than 650 residents and fellows
- Approximately 29,000 admissions, 73,000 emergency department visits, 1.1 million outpatient visits and 33,000 surgical procedures annually
- Designated as a Magnet hospital since 2007
Learn more about Milton S. Hershey Medical Center
Penn State Health Children’s Hospital
600 University Dr., Hershey, Pa. 17033 (Derry Township, Dauphin County)
- An eight-story, 263,000-square-foot-facility built in 2013 and expanded in 2020
- 160 licensed pediatric beds, 26-bed pediatric intensive care unit and a 56-bed neonatal intensive care unit
- Level IV (highest-level) neonatal intensive care unit
- Level I quaternary (highest-level) pediatric intensive care unit
- Level I (highest-level) pediatric trauma center designation
- Intermediate care unit
- Dedicated pediatric operating rooms
- More than 150,000 pediatric outpatient visits, 20,000 pediatric emergency room visits, and approximately 5,000 pediatric patient discharges annually
Welcome to Hershey
More About Hershey
Interested in learning more about living and working in Hershey, Pa.? See details here:
Wellness, including emotional, spiritual, social and physical health, is a crucial component to training and to becoming a professional, compassionate and resilient physician. Self-care is a skill which must be continually practiced and reinforced. Penn State College of Medicine and Penn State Health are committed to addressing wellness among residents and fellows, with multiple resources readily available.
Institutional resources
- Visit BeWell – a health program designed to support Penn State Health employees
- See Penn State College of Medicine wellness resources here
- Employee Health Care Concierge and Case Management Service
- Partners in Medicine
Moving to a new city with your family does not have to be stressful. Residency programs have assisted many significant others with finding employment. There is also a GME-Wide Partners in Medicine (PIM) group that offers networking opportunities as well as various social and community oriented activities. - The Doctors Kienle Center for Humanistic Medicine
- Active and easily accessed Office of Professional Mental Health
Graduate medical education resources
Institutional Resources
Penn State Health and Penn State College of Medicine celebrate, embrace and support the diversity of all patients, faculty, staff, students and trainees.
Office for Diversity, Equity and Inclusion
In keeping with this, Penn State Health has an active Office for Diversity, Equity and Inclusion with various programs, networks and resource groups, including:
- Talks and lectures on diversity, equity and inclusion through the Inclusion Academy
- Regular events on topics such as eradicating racism and creating a culture of inclusiveness
- Many Business Employee Resource Groups (BERGs), including:
- Disability Business Employee Resource Group
- Interfaith Business Employee Resource Group
- LGBTQ+ Business Employee Resource Group
- Military and Veterans Business Employee Resource Group
- Multicultural Business Employee Resource Group
- NextGen Business Employee Resource Group
- Black Physician Professional Staff Association – Resource Group
- Hispanic Professional Association
- Asian Physician and Professional Staff Association
- International Workforce Inclusion
- Inclusion Academy
Learn more about the Penn State Health Office for Diversity, Equity and Inclusion
Learn more about the College of Medicine’s Office for Diversity, Equity and Belonging
Office for Culturally Responsive Health Care Education
The vision at Penn State College of Medicine and Penn State Health is to equip learners with the knowledge, skills and attitudes they will need to provide culturally excellent health care and research for an increasingly diverse U.S. population. The Office for Culturally Responsive Health Care Education was formed to help meet that goal.
Learn more about the Office for Culturally Responsive Health Care Education
Office for a Respectful Learning Environment
In addition, the institution does not tolerate discrimination, biases, microaggression, harassment or learner mistreatment of any kind, and any concerns are immediately addressed by the Office for a Respectful Learning Environment.
Learn more about the Office for a Respectful Learning Environment
Network of Under-represented Residents and Fellows
The Network of Under-represented Residents and Fellows (NURF) is a group of diverse residents and fellows representing all specialties. NURF’s goal is to promote cultural diversity in the residency programs through community involvement, mentorship with diverse faculty, professional networking and support for the recruitment of diverse medical students into the residency programs.
NURF is sponsored by the Penn State College of Medicine Graduate Medical Education Office and the Penn State Health Office for Diversity, Equity and Inclusion.
Curriculum Details
The program will provide training opportunities for a motivated fellow to attain competency to assume the role of medical director of a hematopathology laboratory performing comprehensive, highly complex testing to enable state-of-the-art diagnosis of hematolymphoid disorders.
Fellows will develop communication skills to accurately report results for patient care and to educate their clinical colleagues about rational test ordering and interpretation of results to guide patient care. In addition, the candidate will participate in scholarly activities in order to develop the reasoning skills necessary to critically evaluate the literature and apply this to future practice and/or research endeavors, and if so chosen, to provide a solid foundation for an academic career.
More specifically, the educational goals and objectives of the program will follow the published recommendations of the Society for Hematopathology Education Committee:
Perkins SL, Reddy VB, Reichard KK, Thompsen MA, Dunphy CH; for the Society for Hematopathology Education Committee. Recommended curriculum for teaching hematopathology to subspecialty hematopathology fellows. Am J Clin Pathol. 2007 Jun;127(6):962-76.
There will be only slight modifications to this curriculum based on this institution’s unique institutional resources and experience. Fellows will be provided with this institutional curriculum and provided the Society’s recommended curriculum at the beginning of the training period.
The specific rotational objectives for the rotations included in the fellowship curriculum are outlined on this page and cross-referenced with the ACGME Core Competencies of patient care (PC), medical knowledge (MK), practice-based learning and improvement (PLI), interpersonal and communication skills (ICS), professionalism (P) and systems-based practice (SP).
Upon successful completion of the fellowship program, graduates should:
- I. Have developed sufficient knowledge and skills to assume a position as medical director of a hematopathology laboratory in an academic or private practice setting, overseeing the highly complex testing needed to support evaluation of benign and malignant hematolymphoid disorders involving blood, bone marrow, lymph nodes, spleen and other tissue and cytologic samples (PC, MK, PLI, ICS, P, SP).
- II. Demonstrate good judgment in identifying the limits of their knowledge and skills and the needed for consultation of references and colleagues to assist in the accomplishment of their clinical and academic work (PC, MK, PLI, ICS, P, SP).
- III. Participate in at least one research project related to hematopathology, in order to enhance their skills in critical thinking, evaluation of existing literature, hypothesis generation, experimental design, analysis and writing. This will be important for building skills for lifelong learning (PC, MK, PLI, SP).
I. Introduction to Hematopathology
- Become familiar with the key faculty, staff, locations, processes, procedures and workflow of the Hematology and Special Hematology Laboratories. (PLI, ICS, SP)
- Identify an area of research interest and research mentor. (MK, PLI)
- Review pertinent literature related to research topic. (MK, PLI)
- In collaboration with a research mentor, prepare a research proposal to submit for funding through the Pathology Research Award grant program. (MK, PLI, ICS)
II. Hematology
- Identify age-, gender- and ethnicity-appropriate reference intervals for automated CBC. (PC, MK, PLI, SP)
- Describe the principles and limitations of automated hematology analyzers and apply these concepts to analysis of automated WBC counting and differentials, RBC counting and indices, reticulocyte counting, and platelet counting. (PC, MK, PLI)
- Correctly interpret RBC indices and other laboratory testing to characterize anemias. (PC)
- Correctly identify common abnormalities on body fluid specimens. (PC, MK)
- Correctly identify normal and abnormal morphology RBC, WBC and platelet morphologies on blood films and describe the conditions that may be associated with abnormalities identified. (PC, MK, PLI)
- Identify the appropriate procedures and communicate laboratory results of varying degrees of medical urgency. (PC, MK, PLI, ICS, P, SP)
- Correctly identify morphological abnormalities of white blood cells associated with congenital and acquired disorders, such as: Chediak-Higashi syndrome, May-Hegglin anomaly, Pelger-Huet anomaly, Alder-Reilly anomaly. (PC, MK)
- Correctly identify morphological abnormalities of red blood cells on blood smears associated with congenital and acquired disorders such as: G6PD deficiency, PK deficiency, RBC membrane disorders, abnormal hemoglobins, thalassemias, iron deficiency, megaloblastic anemias, hemolytic anemias, and malaria. (PC, MK)
- Correctly identify morphological abnormalities of platelets associated with congenital and acquired disorders such as: Microangiopathic hemolytic anemias, ITP, gray-platelet syndrome May-Hegglin anomaly. (PC, MK)
- Correctly identify features associated with leukemias: Blasts, lymphoblasts, myeloblasts, Auer rods, CLL, hairy cell leukemia, circulating lymphoma cells, dysplastic features. (PC, MK)
III. Hematopathology
- Bone Marrow: The fellow will use the information obtained from blood smear and bone marrow specimens to diagnose disorders of the hematopoietic systems as listed below.
- Specimen procurement: The fellow will identify indications and contraindications to bone marrow aspiration and biopsy. The fellow will demonstrate appropriate technique while obtaining bone marrow aspiration and biopsy specimens. (PC, MK, PLI, ICS)
- Red blood cell disorders: The fellow will interpret blood and bone marrow findings, in association with pertinent clinical and laboratory information, to correctly diagnose congenital and acquired forms of anemia and erythrocytosis. (PC, MK, PLI)
- White blood cell disorders: The fellow will interpret blood and bone marrow findings, in association with pertinent clinical and laboratory information, to correctly diagnose congenital and acquired disorders associated with eukocytosis or leukopenia (PC, MK, PLI)
- Disorders of platelets: The fellow will interpret blood and bone marrow findings, in association with pertinent clinical and laboratory testing, to correctly diagnose congenital and acquired, benign and neoplastic disorders associated with qualitative and quantitative disorders of platelets. (PC, MK, PLI)
- Bone marrow failure syndromes: The fellow will interpret blood and bone marrow findings, in association with pertinent clinical and laboratory information, to correctly diagnose congenital and acquired, benign and neoplastic disorders associated with bone marrow failure. (PC, MK, PLI)
- Infectious/granulomatous diseases: The fellow will correctly identify morphological features associated with infectious or granulomatous diseases in the bone marrow. (PC, MK, PLI)
- Bone changes: The fellow will correctly identify bone changes associates with primary bone disease, manifestations of systemic diseases and primary hematopoietic disorders. (PC, MK, PLI)
- Neoplastic disorders of the hematopoietic system: Given a patient with a primary hematological disorder the fellow will be able to obtain and synthesize appropriate clinical, morphological, immunophenotypic and genetic data to achieve an correct diagnosis based on the most current accepted system (WHO 2008). (PC, MK, PLI)
- Lymph Node, Spleen, Extranodal Tissues
- Develop a rational approach to handling of tissue specimens suspected of harboring a hematolymphoid disorder, and apply this to triaging and ordering of ancillary studies for surgical and cytological specimens, to optimize the diagnostic and prognostic evaluation. (PC, MK, PLI, SP)
- Understand the normal histology of the lymphatic system, lymph nodes, thymus, spleen, extranodal lymphoid tissues. (MK)
- Be able to diagnose the full spectrum of benign causes of lymphadenopathy, with or without an associated clinical syndrome, and the specific histologic types of lymphomas.
- Know the indications for ordering tests that provide prognostic information and be able to accurately communicate these results to clinical colleagues caring for these patients. (PC, MK, ICS, P, SP)
- Correctly identify non-hematolymphoid neoplasms metastatic to lymphoid organs. (PC, MK)
- Be able to differentiate thymic lymphomas from thymic epithelial neoplasms and thymic hyperplasia. (PC, MK)
- Develop a rational approach to the assessment of primary cutaneous hematolymphoid proliferations and correctly differentiate hematolymphoid neoplasms in the skin from non-neoplastic processes. Be familiar with the types of clinical information that are important for accurate classification of cutaneous hematolymphoid processes. (PC, MK, PLI, ICS, P, SP)
- Develop clinical skill to evaluate congenital and acquired, benign and neoplastic hematolymphoid processes in children, including those processes unique to children and those processes found in both adults and children. (PC, MK, PLI, SP)
- Immunophenotyping and cell cycle analysis
- Flow cytometry
- Correctly describe processing of samples for flow cytometry and applying knowledge of pre-analytical and analytical variables to understanding the limitations of final analysis. (PC, MK)
- Know the criteria for distinguishing between reactive and neoplastic lymphoid proliferations using flow cytometric analysis. (PC, MK)
- Integrate flow cytometric data with additional data, i.e. history, morphology, molecular and cytogenetic data, into comprehensive diagnostic reports for benign and neoplastic lymphoid proliferations. (PC, MK, PLI, ICS, SP)
- Apply flow cytometric data to subclassify and provide prognostic information for lymphomas. (PC, MK, PLI, ICS)
- Integrate flow cytometric data with additional data, i.e. history, morphology, cytochemistry, molecular and cytogenetic data into comprehensive diagnostic reports for benign and neoplastic myeloid proliferations. (PC, MK, PLI, ICS)
- Develop a rational approach to the use of flow cytometry for cytopathology specimens, and know its limitations for the assessment of these specimens.(PC, MK, PLI, SP)
- Apply flow cytometric data to diagnosis of congenital and acquired immunodeficiency states. (PC, MK, PLI)
- Apply flow cytometric data to diagnosis of paroxysmal nocturnal hemoglobinuria-type defect on RBC and leukocytes. (PC, MK)
- Correctly apply consensus guidelines and regulatory guidelines for choosing instrumentation and reagents, validation of assays, assessment of control data, and reporting of results for patient care. (PC, MK, PLI, ICS, P, SP)
- Immunohistochemistry
- Correctly describe processing of samples for immunohistochemistry and apply knowledge of pre-analytical and analytical variables to limitations of final analysis. (PC, MK)
- Develop a rational approach to ordering immunohistochemistry based on clinical history and routine morphology of tissue sections, touch imprints and smears. (PC, MK, PLI, SP)
- Know how to interpret immunohistochemical results and integrate this information with additional information (clinical history, morphology, flow cytometry, molecular and cytogenetic data) into comprehensive reports for tissues with hematolymphoid abnormalities. (PC, MK, PLI)
- Identify common pitfalls related to immunohistochemical testing. (PC, MK, PLI)
- Flow cytometry
IV. Cytogenetics
- Describe the methods used to assess karyotypes of hematological specimens and be familiar with the methods of interpretation. (PC, MK)
- Correctly integrate cytogenetic data into pathology reports for specimens with hematolymphoid disorders, and apply this to diagnosis and prognosis. (PC, MK, PLI, SP)
- Describe the methods and procedures for performing interphase and metaphase FISH, including fresh tissue and fixed tissue. (MK)
- Correctly integrate FISH data into pathology reports for specimens with hematolymphoid disorders and apply this to diagnosis and prognosis. (PC, MK, PLI, ICS, SP)
- Apply knowledge and experience with the methods of karyotyping and FISH to develop a rational approach to ordering and interpreting these studies in the context of hematopathology. (PC, MK, PLI, ICS, SP)
V. Molecular Pathology
- Describe the handling and processing tissues to extract nucleic acids. (MK)
- Describe the methods for evaluating the quality and quantity of extracts. (PC, MK)
- Describe the principles and methods of Southern blotting, PCR, reverse transcription-PCR and real-time PCR and evaluate the relative strengths and weaknesses of various detection methods. (PC, MK, PLI)
- Describe the indications, technique, analysis and limitations of common tests in hematopathology: (PC, MK, PLI, SP)
- TCR gene rearrangements: Southern blot, PCR
- Immunoglobulin gene rearrangements: Southern blot, PCR
- EBV clonality: Southern blot
- Translocation product detection (BCR/ABL1, PML/RARA, IGH/BCL2, etc): PCR, RT-PCR
- Quantitation of BCR/ABL1 for minimal residual disease
- Identification of infectious agents, e.g., HHV8, parvovirus B19, HTLV1, M. tuberculosis, B. henselae
- Mutation detection: JAK2, Flt3, NPM, hemochromatosis, coagulopathies
- Identify appropriate QA and QC procedures for molecular testing and apply this to identifying sources of potential false-positive or false-negative results. (PC, MK, PLI, ICS, P, SP)
- Develop a rational approach to ordering molecular testing in the context of hematopathology. (PC, MK, PLI, SP)
- Correctly integrate molecular data with additional information such as clinical history, morphology, immunophenotype, and cytogenetics results into comprehensive reports for specimens with hematolymphoid processes. (PC, MK, PLI, SP)
- Describe the principles of gene-chip arrays and interpretation of data. (PC, MK, PLI)
VI. Coagulation
- Describe the background, procedure, and limitations of routine coagulation tests, such as PT, PTT, TT, reptilase time. Correctly interpret these data at sign-out rounds and identify sources of potentially misleading results. (PC, MK, PLI, SP)
- Develop a rational approach to the workup of abnormal PTT and PT. (PC, MK, PLI)
- Describe the background, procedures and limitations of factor and inhibitor assays and suggest appropriate factor replacement. (PC, MK, PLI)
- Describe the defects associated with von Willebrand disease, clinical features, laboratory diagnosis and treatments. (PC, MK, PLI, SP)
- Develop a rational, evidence-based approach to evaluation and laboratory testing for patients with platelet disorders. (PC, MK, PLI, SP)
- Develop a rational, evidence-based approach to the clinical and laboratory evaluation of patient with a suspected risk of thrombosis. (PC, MK, PLI, SP)
- Develop a rational approach to evaluation and laboratory testing of patients with microangiopathic hemolytic anemias such as, DIC, TTP, and mechanical fragmentation. (PC,
MK, PLI, SP) - Describe the principles, QA/QC and interpretation of tests to monitor anticoagulation. (PC,
MK, PLI, SP) - Integrate clinical history, physical examination and laboratory testing in the context of patients with disorders of coagulation, and generate comprehensive consultations for patients with disorders of coagulation. (PC, MK, PLI, ICS, P SP)
VII. Laboratory Management
This material is covered in the other rotations and in lectures.
- Select appropriate internal and external QA/QC procedures for hematology laboratory testing. (PC, MK, PLI)
- Analyze QA/QC data obtained from the hematology laboratories. (PC, MK, PLI)
- Evaluate various resources for intramural and extramural proficiency. (PC, MK, PLI, SP)
- Describe how pre-analytical and analytical factors may be optimized in various hematology tests. (PC, MK, PLI)
- Develop a rational approach to selecting reference laboratories for testing that is impractical on site. (PC, MK, PLI, ICS, P, SP)
- Communicate effectively with clinical colleagues about selection and interpretation of tests. (MK, ICS)
- Understand billing and reimbursement procedures for hematology testing. Apply appropriate coding to tests.
- Successfully complete at least one formal quality project, and present results at the annual Departmental Quality Improvement forum. (PC, MK, PLI, ICS, SP)
- Understand the requirements of accrediting bodies (College of American Pathologists and others) for accreditation of the hematology laboratories. (PC, PLI, SP)
Intro to Hematology
Time: Two weeks
Educational Focus: During the first two weeks of the fellowship period, Dr. Bayerl will introduce the fellow to the personnel, PSHMC facilities, and routine workflow of the hematopathology service, department and institution. The fellow will be asked to choose a research mentor and select a research project with their mentor. Depending on the fellow’s prior research experience and area of research interest, the fellow may select a research mentor from among the hematopathology Faculty, faculty in the Division of Experimental Pathology or investigators in Adult or Pediatric Hematology/Oncology.
Supervising Faculty: Michael Bayerl, MD
Key Facility: Penn State Health Milton S. Hershey Medical Center
Hematopathology
Time: 25 weeks
Educational Focus: This rotation deals with the evaluation of hematolymphoid malignancies and other atypical proliferations, in bone marrow, lymph nodes, spleen, extranodal sites and blood and body fluids sent for flow cytometric analysis. The 25-week rotation is divided into several blocks, with other rotations interspersed. Drs. Bayerl, Malysz and George are responsible for evaluation and interpretation of all of these cases and for the supervision/education of trainees.
Sample accessioning is performed in Surgical Pathology (tissues), the Cytopathology Laboratory (body fluids), the Special Hematology Laboratory (all cases sent for flow cytometric analysis) and the Diagnostic Molecular Laboratory (cases sent for inhouse molecular testing). Review of the slides and other laboratory results takes place daily in a dedicated Hematopathology Sign-Out Room, which is equipped with a multiheaded microscope, digital camera, flat screen projection, two PC workstations and reference books.
Didactic presentation by the faculty, study sets, directed reading and online resources will assist in covering rare conditions and testing that is not performed on-site.
Bone Marrow: The Fellow will be intimately involved in all aspects of bone marrow evaluation including gathering of pertinent clinical information; evaluating complete blood cell counts and morphology on peripheral blood specimens; examination of aspirate smears and biopsies; triaging specimens for ancillary testing (e.g., cytogenetics, flow cytometry, histochemistry, immunohistochemistry, microbiology studies and molecular testing) based on initial history and blood and bone marrow findings. The institution emphasizes generating comprehensive bone marrow reports that incorporate all of the above testing, as indicated, into a single report that facilitates clear communication of the results to clinical colleagues. An Adult or Pediatric Hematology/Oncology Fellow is usually present at sign out rounds and plays an active role in the process by providing clinical information about patients. This enhances the learning experience for the trainees, providing additional experience in system-based practice.
Although the majority of bone marrow aspirate and biopsy procedures are performed by faculty and fellows from the Divisions of Adult and Pediatric Hematology/Oncology, the faculty in these divisions teaches pathology trainees to perform the procedures on patients. Fellows are responsible to arrange training in bone marrow aspirations and biopsies during their hematopathology rotation. The fellow will read reading list resource 7, Chapter 3 (Foucar), and view other resource video 1, before contacting the Nurse Practitioners or Physician Assistants in the day clinic to arrange notification for performance of bone marrow procedures.
Procedure: The fellow (trainee) will contact Susan Rokita, CRNP, at pager 1193 or 717-531-4627 (or Hoang Dinh, CRNP), to schedule procedures. Ms. Rokita and her staff will familiarize he trainee with their specific procedures. The trainee will observe at least one procedure by the NP or PA (Mid-Level) before performing the procedure. When the Mid-Level is comfortable with the trainee’s observation, the trainee will be able to perform procedures under the direct supervision of the NP or PA. The fellow will perform a minimum of five to 10 procedures under the direct supervision of the Mid-Level until judged as competent. Once the fellow is found to be competent, he/she will no longer be required to attend or perform bone biopsy procedures. The “procedure” will include: Review patient’s record to determine valid order, indication, absence of contraindication and specimens to be obtained; soliciting informed consent; technical performance of the procedure and post-procedure review with the supervising Mid-Level. The trainee will never perform a bone marrow procedure without direct supervision by a Mid-Level or Hematology/Oncology attending physician.
Documentation: Record of performance of bone marrow procedures should be documented by completing the bone marrow aspirate/biopsy log, available in the Fellowship Handbook.
Lymph Node, Spleen, Extranodal Tissues: All specimens from the Surgical Pathology and Cytopathology services, which contain hematopoietic or lymphoid neoplasms or atypical lymphoid proliferations, are accessioned to, evaluated by, and interpreted by the hematopathology faculty.
Under the guidance of the faculty, the fellow will develop competency in all aspects of pathological evaluation of lymph node, spleen and hematolymphoid processes in extranodal tissues, including obtaining pertinent clinical history, gross examination, triage of tissues for optimal diagnostic evaluation, microscopic examination, and integration of information from ancillary studies (immunohistochemistry, flow cytometry, gene rearrangement studies, in situ hybridization, and cytogenetic studies). Emphasis will be placed on creating a single integrated report that contains all pertinent data from the testing performed. Communication and interdisciplinary interactions will be facilitated by communal sign out rounds involving faculty and trainees from Adult and Pediatric Hematology/Oncology and through weekly meetings of the Penn State Cancer Institute Hematological Malignancies Team which includes the hematopathologists and hematology/oncology faculty.
Ancillary Studies: The fellow will be directly involved in deciding which ancillary testing is appropriate, if any, for all blood, bone marrow, lymph node, spleen and extranodal tissue specimens. Immunohistochemistry, in situ hybridization, flow cytometry and other types of molecular diagnostic testing are performed on site. Easy access to the laboratories performing the testing facilitates reviewing the primary data in correlation with the morphology, an optimizing the evaluative processes. Through hands-on participation in this process, the fellow will learn to choose the appropriate techniques for evaluation of the full spectrum of hematolymphoid abnormalities, as well as the intricacies of interpretation and the limitations of these tests. In-house interpretation of select FISH panels is performed by the fellow and supervising faculty. Karyotyping, sendout FISH studies, and send-out molecular testing are performed at the Mayo Medical Laboratories. The fellow will also have a one- to two-week rotation at Quest Diagnostics for hands-on experience in cancer cytogenetics testing.
Supervising Faculty: Michael Bayerl, MD; Jozef Malysz, MD; Melissa George, DO
Key Facility: Penn State Health Milton S. Hershey Medical Center
Research
Time: Two weeks
Educational Focus: This block will provide protected time to initiate or complete a small research project, or to make substantial progress on a more ambitious project. The main supervising faculty will be the mentor chosen by the fellow for the research project. The fellow will have access to use any Penn State Health Milton S. Hershey Medical Center facility, including the Pathology Core Reference Laboratory.
Supervising Faculty: Michael Bayerl, MD
Key Facility: Penn State Health Milton S. Hershey Medical Center
Hematology
Time: Four weeks
Educational Focus: This portion of the curriculum deals with testing performed in the hematology section of the Clinical Laboratory. Dr. Donaldson, Medical Director of Hematology and Thrombosis, will be the primary faculty member responsible for overseeing this portion of the curriculum, with other members of the Clinical Pathology Division participating on a rotating basis. The fellow will become familiar with the indications, technologies, and limitations of routine testing of blood and body fluid samples for the evaluation of hematologic disorders.
The fellow will develop competence in microscopic evaluation and interpretation of blood and body fluid samples, through daily participation in sign out rounds. Microscopic review will be performed in conjunction with review of other clinical laboratory test results as appropriate for the clinical and laboratory problem being evaluated. Testing covered in this portion of the curriculum includes review of blood smears, body fluids, hemoglobin evaluations and coagulation testing. Daily sign out rounds will occur in the Clinical Pathology Residents’ office, at a multiheaded microscope with camera, flat screen projection, and Cellavision. Several PC workstations are also available in the residents’ room and in the Automated Testing Laboratory.
Direct observation of automated analyses and hands-on bench experiences will be encouraged. The fellow will also learn to apply principles of Quality Assurance and Quality Improvement in the context of hematology testing. The Hematology Laboratory performs approximately 150,000 complete blood counts with white blood cell differential counts annually, of which 525 require review by residents and faculty. More than 3,400 body fluid specimens are analyzed, including 2,300 CSF, 800 serous fluids, and 260 bronchoalveolar lavage fluids. More than 160 of these specimens per year require review by residents and faculty with the generation of interpretive reports. Approximately 200 hemoglobin capillary electrophoresis and 600 coagulation interpretations are generated annually. Didactic presentations by the faculty, study sets, directed reading and online resources will assist in covering rare conditions and testing that is not performed on site.
Supervising Faculty: Diana Desai, MD, and Michael Creer, MD
Key Facility: Penn State Health Milton S. Hershey Medical Center
Coagulation
Time: Four weeks
Educational Focus: The fellow’s training in coagulation will stress integration of clinical data and interpretation of coagulation laboratory test results. The fellow will actively participate in the interpretation of laboratory coagulation studies and in clinical consultations for coagulopathies. The fellow will see patients in hemophilia clinic under the supervision of hematologists specializing in disorders of hemostasis and thrombosis. These patient consultations will foster communication with clinical colleagues and develop direct patient-care skills. The fellow will be required to attend the established didactic series on disorders of coagulation and laboratory testing. This is provided by faculty of the Divisions of Hematology/Oncology and Pathology. Study sets, directed reading and online resources will assist in covering rare conditions and testing that is not performed on site. Dr. Donaldson will supervise this portion of the fellow’s training.
Supervising Faculty: Diana Desai, MD, and Michael Creer, MD
Key Facility: Penn State Health Milton S. Hershey Medical Center
Cytogenetics
Time: Two weeks
Educational Focus: Cytogenetics is a crucial diagnostic and prognostic tool in hematopathology. The fellow will spend two weeks at Quest Diagnostics Nichols Institute, Chantilly, Virginia, to learn the basic principles, techniques and limitations of karyotype and FISH analyses as they are applied to hematopathology. Given the reference laboratory’s generous facilities, fellows will participate in bench work to learn the important steps leading to the generation of information for relevant studies. The fellow will also participate in the interpretation of active cases. The knowledge gained in this rotation will enhance the fellow’s understanding of the meaning of test results from outside laboratories, which are reported on in-house cases, and will enhance their ability to triage cases for cytogenetic studies.
Molecular
Time: Four weeks
Educational Focus: Molecular pathology techniques are increasingly important to the practice of hematopathology. During this rotation, the fellow will develop a basic understanding of molecular pathologic testing and its uses, limitations and costs, with particular emphasis on tests related to hematopathology. The curriculum will cover basic concepts in molecular biology and pathology including nucleic acid structure, gene regulation and function, and mechanisms of inherited and acquired mutations. Hands-on experience in the performance of the testing will be included. Fellows will learn the techniques of DNA and RNA extraction and purification, reverse transcription, PCR, RT-PCR, quantitative real-time PCR, Invader technology, and capillary electrophoresis. The fellow will learn to interpret molecular test results from blood, marrow and tissue and correlate them with standard pathologic techniques; these assays will include tests for BCR ABL, PML RARA, JAK2, factor V Leiden, prothrombin G20210A, and TCR and IgH gene rearrangements. QA/QC considerations involved in running a molecular laboratory will also be discussed. Dr. Donaldson will supervise the fellow.
Supervising Faculty: Guoli Chen, MD, PhD, and Rinal Kansal, MD
Key Facility: Penn State Health Milton S. Hershey Medical Center
Electives (such as Benign Hematology, Molecular, Coagulation)
Time: Four weeks total
Educational Focus: This time will be used by the fellow to provide additional experience in an area of interest or on research.
Supervising Faculty: Michael Bayerl, MD, and/or lead faculty in area of selected elective.
Key Facility: Penn State Health Milton S. Hershey Medical Center
Continuing Medical Education
Time: One week
Educational Focus: The fellow will be strongly encouraged to attend a scientific/professional meeting to enhance knowledge about current advances in hematopathology. The institution provides $1,000 to offset the cost of the travel.
Supervising Faculty: Michael Bayerl, MD
Fellows are expected to attend and present at the annual Atlantic Regional Hematopathology meeting during their fellowship.
Travel expenses associated with attendance at professional meetings are eligible to be reimbursed from the annual fellow stipend. For fellows who are presenting posters or podium presentations at meetings, additional financial support can be requested from the Pathology Research Initiation Grant (RIG) program.
If the fellow’s attendance at a meeting is contingent upon obtaining this additional support, then approval of the additional funding must be obtained from the Pathology RIG Committee prior to submitting an abstract or agreeing to make a presentation.
Institutional policies apply in the Hematopathology Fellowship. Where program-specific policies exist, they are listed below.
Supervision: Hematopathology
The Program Director ensures appropriate supervision of the fellow by the teaching faculty by direct observation, through discussions at monthly meetings with the fellow and confidential evaluations submitted by the fellow.
Two weeks of training will be at Quest Diagnostics Nichols Institute, Chantilly, Virginia, under the supervision of Daniel Jones, MD, PhD. Details of supervision are prescribed in the letter of agreement. Direct feedback will be solicited from the fellow regarding supervision during this rotation.
The institution has established the lines of responsibility for supervision. The fellow is supervised by the attending physician on the service, and this attending physician is supervised by the Program Director (for educational performance) and by the Division Chief and Chair (for clinical and educational performance).
On-Call: Hematopathology
Hematopathology fellows will not be expected to take call.
Required Texts
The following texts are required reading for the Hematopathology Fellowship.
- Perkins SL, Reddy VB, Reichard KK, Thompsen MA, Dunphy CH; for the Society for Hematopathology Education Committee. Recommended curriculum for teaching hematopathology to subspecialty hematopathology fellows. Am J Clin Pathol. 2007 Jun; 127(6):962-76.
- Beutler E, Lichtman MA, Coller BS, Kipps TJ, Seligsohn U. Williams Hematology. 6th edition. New York: McGraw-Hill. 2001.
- Brunning RD, McKenna RW. Atlas of Tumor Pathology: Tumors of the Bone Marrow. Washington, DC: Armed Forces Institute of Pathology; 1994.
- Carey JL, McCoy JP, Keren DF. Flow Cytometry in Clinical Diagnosis. 4th edition. Chicago: American Society for Clinical Pathology Press; 2007.
- Cerroni L, Gatter K, Kerl H. An Illustrated Guide to Skin Lymphoma. 2nd edition. Massachusetts: Blackwell Publishing Inc; 2004.
- Farhi DC, Chai CC, Edelman AS, Parveen T, and Vo TLT. Pathology of Bone Marrow and Blood Cells. Philadelphia: Lippincott Williams & Wilkins; 2004.
- Foucar K. Bone Marrow Pathology. 3rd edition. Chicago: American Society of Clinical Pathologists; 2010.
- Glassy EF. Color Atlas of Hematology: An Illustrated Field Guide Based on Proficiency Testing. Illinois: College of American Pathologists; 1998.
- Gorczyca W. Flow Cytometry in Neoplastic Hematology. London: Informa Healthcare; 2006
- Gulati G, Caro J. Blood Cells: An Atlas of Morphology. Chicago: American Society for Clinical Pathology Press; 2007.
- Hoffbrand AV, Pettit JE. Color Atlas of Clinical Hematology. 3rd edition. London: Mosby; 2000.
- Henry JB. Clinical Diagnosis and Management by Laboratory Methods. 20th edition. Philadelphia: WB Saunders Company. 2001.
- Hoyer JD, Kroft SH. Color Atlas of Hemoglobin Disorders: A Compendium Based on Proficiency Testing. Chicago: CAP Press, 2003.
- Hsi ED. Hematopathology: a volume in the series Foundations in Diagnostic Pathology, Philadelphia, Elsevier; 2007.
- Ioachim HL, Medeiros LJ. Ioachim’s Lymph Node Pathology. 4th edition. Philadelphia: Lippincott Williams & Wilkins; 2008.
- Jaffe ES. Surgical Pathology of the Lymph Nodes and Related Organs. 2nd edition. Philadelphia: WB Saunders Company; 1995.
- Kitchens CS, Alving BA, Kessler CM, Applegate AJ. Consultative Hemostasis and Thrombosis. 2nd Edition. Philadelphia: WB Saunders Company. 2007.
- Kjeldsberg CR. Practical Diagnosis of Hematologic Disorders, 1 Benign Disorders. 4th edition. Chicago: American Society for Clinical Pathology Press; 2006.
- Kjeldsberg CR. Practical Diagnosis of Hematologic Disorders, 2 Malignant Disorders. 4th edition. Chicago: American Society for Clinical Pathology Press; 2006.
- Knowles DM. Neoplastic Hematopathology. 2nd edition. Philadelphia: Lippincott Williams & Wilkins. 2001.
- Orazi N. Disorders of the Spleen. 2nd edition. Philadelphia: WB Saunders Company; 1999.
- Lee GR, Foerster J, Lukens J, Paraskevas F, Greer JP, Rodgers GM. Wintrobe’s Clinical Hematology. Vol 1. 10th edition. Philadelphia: Lippincott Williams & Wilkins. 1999.
- Lee GR, Foerster J, Lukens J, Paraskevas F, Greer JP, Rodgers GM. Wintrobe’s Clinical Hematology. Vol 2. 10th edition. Philadelphia: Lippincott Williams & Wilkins. 1999.
- McClatchey K. Clinical Laboratory Medicine. 2nd Edition. Philadelphia: Lipincott Williams & Wilkins, 2002.
- Nathan DG, Orkin SH, Ginsburg D, Look AT. Nathan and Oski’s Hematology of Infancy and Childhood, Vol 1. 6th edition. Philadelphia: WB Saunders Company; 2003.
- Nathan DG, Orkin SH, Ginsburg D, Look AT. Nathan and Oski’s Hematology of Infancy and Childhood, Vol 2. 6th edition. Philadelphia: WB Saunders Company; 2003.
- Sun T. Flow Cytometric Analysis of Hematologic Neoplasms: A Color Atlas & Text. 2nd edition. Philadelphia: Lippincott Williams & Wilkins; 2002.
- Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. 4th edition. Lyon: IARC Press. 2008.
- Torlakovic EE, Naresh KN, Brunning RD. Bone Marrow Immunohistochemistry. Chicago: American Society for Clinical Pathology Press; 2009.
- Coleman WB, Tsongalis GJ. Molecular Diagnostics for the Clinical Laboratory, 2nd Edition, Tetowa, New Jersey: Human Press Inc. 2006.
- Warnke RA, Weiss LM, Chan JKC, Cleary ML, Dorfman RF. Atlas of Tumor Pathology: Tumors of the Lymph Nodes and Spleen. Washington, DC: Armed Forces Institute of Pathology; 1995.
- Weiss LM. Lymph Nodes (Cambridge Illustrated Surgical Pathology). New York: Cambridge University Press; 2008.
Other Resources
- Video in Clinical Medicine: Bone Marrow Aspiration and Biopsy by Suman Malempati, MD, Sarita Joshi, MD, Susanna Lai, MPH, Dana A.V. Braner, MD, and Ken Tegtmeyer, MD, in N Engl J Med 2009; 361:e28 October 8, 2009.
Latest News from Pathology
Jan. 9, 2025
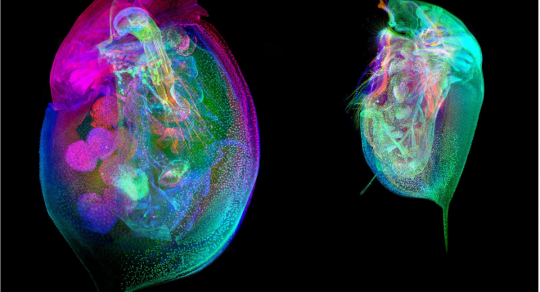
Revolutionizing environmental research: First Daphnia Histology Reference Atlas published

Dec. 6, 2024
Rojiani wins lifetime achievement award from the College of American Pathologists

Nov. 4, 2024
Rojiani honored with 2024 College of American Pathologists Lifetime Achievement Award
Oct. 22, 2024
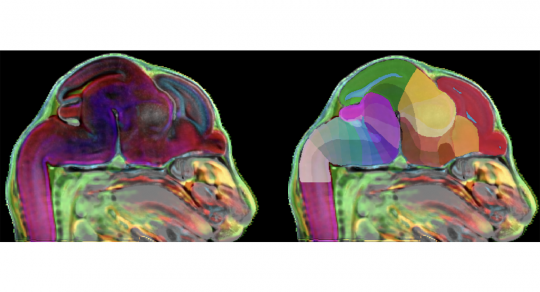
Researchers develop 3D atlas of the developing mammalian brain